Antipyretics for children are prescribed by a pediatrician. But there are emergency situations for fever when the child needs to be given medicine immediately. Then the parents take responsibility and use antipyretic drugs. What is allowed to give to infants? How can you bring down the temperature in older children? What medicines are the safest?
Almost every year, patients come in who have not been diagnosed in a timely manner with subcutaneous ruptures of the extensor tendons of the fingers. Closed injuries of the extensor tendons of the fingers are observed at various levels, but most often in the area of the distal interphalangeal joint, i.e., at the site of attachment of the extensor apparatus and in the area of the proximal interphalangeal joint.
N. I. Pirogov (1843) noticed the functional unity of the common extensor of the fingers and the intrinsic muscles of the hand, which form the dorsal aponeurosis or extensor apparatus of the finger. The dorsal aponeurosis has the shape of a triangular plate, the top of which is attached to the distal phalanx, and the corners of the base are directed to the sides and proximally (Fig. 89).
The tendon of the common extensor of the fingers at the level of the proximal phalanx is divided into three bundles. The central bundle crosses the proximal interphalangeal joint and attaches to the base of the middle phalanx. The lateral parts of the common extensor tendon converge, merge into one bundle, which crosses the distal interphalangeal joint and attaches to the base of the distal phalanx. At the level of the metacarpophalangeal joint, the fascia of the rear of the finger forms transversely extending bundles.
Their distal part, which has an arcuate course, unites the tendon of the common extensor of the fingers with the fibers of the tendons of the own muscles of the hand that come to it from the sides. In this case, a kind of "hood" is formed, covering the joint from the rear and from the sides. When the finger moves, the "hood" slides freely over the back surface of the proximal interphalangeal joint.
Rice. 89. The extensor apparatus of the finger (according to N. I. Pirogov).
1 - opened bone-fibrous canal of the finger; 2 - tendon of the deep flexor of the fingers; 8 - a loop formed by splitting the tendon of the superficial flexor of the fingers; 4 - mesentery of the tendon; 5 - tendon of the common extensor of the fingers; c - tendons of interosseous and worm-like muscles; 7 - intertendon joints of the extensor apparatus of the finger.
In case of violation of the integrity of the central bundle of the extensor tendon with a rupture of the triangular ligament, the lateral fibers of the tendon are displaced to the palmar side. The head of the proximal phalanx protrudes through the resulting gap between the divergent lateral bundles of the extensor tendon (Fig. 90). The subsequent wrinkling of the lateral sections fixes the middle phalanx in the flexion position, and the distal phalanx in extension; there is a "symptom of the loop" - the so-called double contracture of the finger.
It must be constantly remembered that only flexion of the finger provides relaxation of the extensor apparatus. Fixation of the finger in an extended position in the treatment of injuries of the extensor apparatus is the most common mistake. For a differential diagnosis, it must be remembered that sprains in the distal interphalangeal joint of the fingers are rare, and contusions and extensor tears are more frequent. Therefore, an X-ray examination is always necessary.
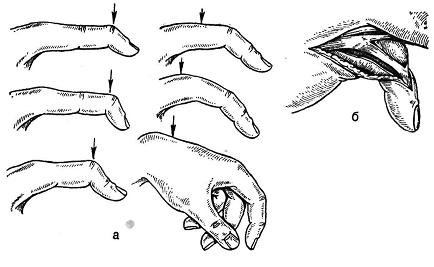
Rice. 90. The characteristic position of the finger depending on the level of damage (indicated by an arrow) of the extensor tendon (a); splitting of the dorsal aponeurosis of the finger at the level of the proximal interphalangeal joint with subluxation of the middle phalanx of the fifth finger (b).
There are two types of subcutaneous rupture of the extensor apparatus of the finger at the level of the distal interphalangeal joint: rupture without damage and with bone damage, incomplete and complete. With the first, incomplete extensor movements of the distal phalanx are possible. With the second, extension is impossible, a "finger-hammer" is formed.

Rice. 91. Fixation of the distal interphalangeal joint with a metal plate with an adhesive plaster and a plaster cast (a, b); fixing the finger in the "writing" position (c); operation - suture of the extensor tendon (d).
Recognition of a subcutaneous rupture of the extensor tendon of the finger is not difficult if the surgeon pays due attention to the history and examination of the patient. This type of injury occurs more often after a sudden butt blow to the finger or direct support on the finger. In this case, the finger acquires the position and shape characteristic of a tendon rupture, and a corresponding loss of the extension function occurs - these are signs by which one can judge the level of damage to the extensor apparatus (see Fig. 90).
Treatment of subcutaneous ruptures of the extensor tendons. With regard to the treatment of subcutaneous injuries of the extensor tendons, there is currently no single view. Many authors recommend the use of surgical treatment - tendon suture with subsequent immobilization of the phalanx; other surgeons believe that good and at least not worse results can be achieved with conservative treatment. We adhere to this opinion in relation to subcutaneous ruptures of the extensor at the level of the distal interphalangeal joint. For ruptures in the area of the proximal joint, we consider surgical treatment indicated.
The success of conservative treatment of closed extensor injuries in the area of the distal interphalangeal joint depends on timely recognition and complete immobilization of the finger. Having tried various methods and the timing of fixation and comparing the results, since 1938 we have been using immobilization of the finger in the "writing" position - extension in the distal and flexion in the proximal interphalangeal joint (Fig. 91) - for 4-6 units (E. V. Usoltseva, 1939). Fixation is carried out with a back gypsum, colloidal or sticky bandage, less often with a Kirschner wire. In elderly people suffering from age-related and metabolic changes in the interphalangeal joints, we limit ourselves to applying a splint in a half-bent position of the finger. For patients whose work requires differentiated movements of the distal phalanx, if immobilization fails, surgery is recommended.
Currently, surgeons continue to explore new ways to suture, secure, and hold the extensor tendon until it heals. Preference is given to internal splinting with a spoke and the Bennel method. The distal and proximal ends of the extensor are sutured with stainless steel wire or nylon thread. The ends of the thread are brought out distally and tied over the button. If necessary, the seam is supplemented with single seams from the sides, the integrity of the joint capsule is restored. After 3-4 weeks, the sutures are trimmed and pulled out. Immobilization of the finger is achieved with a plaster bandage or a transosseous Kirschner wire. When a tendon is torn with a bone fragment, a transosseous suture is used.
In case of damage to the extensor aponeurosis of the finger at the level of the proximal interphalangeal joint, various methods of tendoplasty are also offered in order to bring together the separated lateral bundles of the extensor tendon. Damage to the extensor tendon at the level of the proximal interphalangeal joint was studied by V. G. Vainshtein (1958). The purpose of the operation is to correct the deformity and restore the extensor apparatus of the finger. Correction is achieved after the allocation and restoration of the ratio of the lateral bundles, polerical and oblique fibers of the aponeurosis.
Most surgeons here and abroad believe that fresh subcutaneous injuries of the extensor tendons should be treated conservatively. The reason for the failures lies in non-compliance with the basic principles of the treatment of these injuries. The main mistakes include fixation of the injured finger in the extension position in the proximal interphalangeal and metacarpophalangeal joints and insufficient immobilization period - less than 4 weeks.
Operations should always be preceded by the elimination of stiffness and stiffness of the joints of the hand and an examination of the patient's state of health. The results of surgical restoration of the extensor apparatus at the level of the proximal interphalangeal joint are better than in the area of the distal joint. In the literature, there are isolated reports of more rare cases of subcutaneous injuries of the extensor tendons. thumb, own extensor of the II finger and other formations of the extensor apparatus.
E.V.Usoltseva, K.I.Mashkara
Surgery for diseases and injuries of the hand
The main instrument of man tends to be damaged due to its thin and complex structure and constant exposure to dangerous situations. Of course, we are talking about the hands, or rather, the hands. Alas, damage tendons of fingers by no means uncommon. The bridges between muscle tissue and bones are torn due to the fact that the tendon, due to its anatomical structure, not able to stretch, as it does not have elasticity. Finger tendon rupture is tantamount to losing an entire finger. And if with an injury to the little finger only 8% of the function of the hand falls out, then with damage to the thumb - all 40%. It is not difficult to assess the seriousness of this problem even for a person without a medical education.
Classification of finger tendon injuries
- Depending on whether there is a violation of the integrity of the skin, open and closed injuries of the hand are distinguished. Closed, in turn, are divided into traumatic and spontaneous, when the cause is unknown, or rather, it lies inside, in degenerative changes.
- The number of damaged tendons of fingers isolated (single) and multiple injuries. If there is damage to other structures - muscles, bones, blood vessels, nerves - the injury is called combined.
- The nature and strength of the traumatic agent determines whether a partial or complete rupture occurs.
- The timing of the presence of an existing hand problem is taken into account when dividing finger tendon injuries for fresh (0-3 days), stale (4-20 days) and old (3 weeks or more).
Finger flexor tendon ruptures
Patients come to us with complaints about the violation of the activity of one or another finger. The pain may go away, but the inability to bend the finger remains, which makes you come to the doctor. The hand has two muscles that flex the fingers, however, one of which lies deep, and the other is superficial. To identify whether the tendons are damaged and which ones, a simple diagnostic procedure is performed.
- If your nail phalanx does not bend, then the deep flexor of the fingers is injured.
- If, with a fixed main (first) phalanx, the other two do not bend, then they are hurt tendons both flexor muscles fingers of the hand. The ability to bend a straight finger remains, since small interosseous and vermiform muscles are responsible for this.
- If only the superficial flexor of the fingers is damaged, then the function of the finger is not impaired, because its work is compensated by the deep flexor.
Treatment consists only in carrying out the operation. In the acute period, the doctor will try to stitch the tendon. There are many types of tendon sutures, many of which our surgeons are proficient in. In case of chronic damage or ineffectiveness of the performed operation, tendoplasty is performed - replacement of the tendon with a graft. After injury tendons of the fingers that bend them, need a immobilizing bandage on the hand and forearm for 3 weeks.
Finger extensor tendon injury
The anatomy of the extensor fingers is somewhat different. A tendon departs from the finger extensor muscle. It is divided into 3 parts: the central one is attached to the main phalanx, and the two side ones are attached to the nail. Thus, the result of the injury will directly depend on which portion of the tendon is damaged. If these are the lateral parts, then the patient cannot straighten the nail phalanx and the finger looks like a hammer. When the central portion is affected, hyperextension of the distal interphalangeal joint is observed. Such a finger is figuratively called a "boutonniere". If the damaged area tendons of fingers lies higher, the finger assumes a bent position and the person is not able to unbend it on his own.
Due to the fact that the ends tendons extensors fingers of the hand do not diverge far, you can achieve their fusion without surgery by applying a plaster cast. Each level of damage has its own fixation position. However, we cannot reliably know whether the ends of the tendons have grown together, whether there are conditions for this, therefore, today operational tactics are preferred.
Of course, the article on the site is not a guideline for you to make a diagnosis yourself. In any case, a doctor's consultation is required. Traumatologists in medical center GarantClinic develop such a direction as hand microsurgery and accept patients with finger tendon ruptures. We use technologies that meet European standards to perform complex labor-intensive operations on the hand, and ours are available to all segments of the population.
The relevance of the topic of tendon injuries does not require evidence, if only because approximately 28-28% of all injuries of the hand and fingers are accompanied by tendon injuries. The duration of rehabilitation treatment after tendon injuries reaches 8-12 months, which is comparable in terms of labor loss with the most severe injuries of the musculoskeletal system. At the same time, the administration of medical institutions still maintains a superficial attitude towards tendon injuries, which entails a reduction in the complexity of operations, an unreasonable reduction in the bed-day for these patients, numerous violations in rehabilitation programs towards their reduction, etc. .
Statistics and classification
The statistics of damage to the structures of the hand are covered in different ways in the literature. Without delving into the subtleties, you should know that the flexor tendons of the fingers are most often damaged. In second place are the same injuries, but in combination with damage to the nerves of the fingers and hand.
The third most common injury is to the extensor tendons at different levels- from the fingertips to the middle third of the forearm. Localization of damage to the flexor tendons of the fingers is possible at any level. From an anatomical point of view, the structure of the tendon is the same throughout. On different fingers, it differs mainly in the cross-sectional area and in some areas in the shape of this section. At the same time, surgical restoration of tendons at different levels of the hand has distinctive features. The practical experience of plastic surgeons has shown that, depending on the characteristics of the flexor tendon repair technique and postoperative rehabilitation treatment it is advisable to allocate 5 zones of damage.
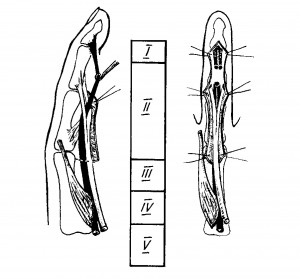
Rice. 1 Scheme of dividing the flexor tendons into zones
Areas of damage to the flexor tendons.
Treatment of isolated injuries of the flexor tendons of the hand and fingers in combination with damage to the neurovascular bundle is a difficult problem in hand surgery. However, the most complex type of injury is considered to be a combination of bone fractures with damage to all soft tissue structures. Incomplete detachment is considered damage to the finger (fingers) or hand by more than half of the cross section with a break in blood vessels and nerves, as well as detachment, in which any connection of the damaged part of the segment with the segment itself is preserved; complete - when the detached part of the segment has no connection with the rest.
ORGANIZATION OF TREATMENT
Treatment of victims with damage to the tendons, neurovascular bundles, especially in combination with fractures of the bones of the hand, should be carried out only in specialized medical institutions and, as an exception, in an ordinary hospital, with a trained specialist, special equipment and facilities. The list is minimal necessary equipment should include:
- Operating table.
- Side table for operations on the upper limb.
- Shadowless lamp and side light.
- operating microscope.
- Binocular head-mounted magnifier with fiber illuminator.
- Chairs with adjustable seat height.
- Sterile linen in sufficient quantity.
- Diathermocoagulator bipolar with tips.
- Microcoagulator for small vessels.
- Pneumatic cuffs with pressure gauge for pressure adjustment.
In addition to general surgical instruments, the list of necessary equipment should include:
- Sterile disposable scalpels with handles.
- Tweezers are anatomical, surgical, microsurgical.
- Hooks of small and medium size.
- Probes are button-shaped, grooved, with a loop.
- Raspator straight and grooved different sizes.
- Chisels of small sizes.
- Small bone nippers.
- Hammer 50 gr. with a handle.
- Drill manual inertialess small sizes with a set of drills.
- Kirschner spokes.
- Titanium wire in coils.
- Atraumatic needles of different sizes.
- Suture material from #5/0 to #10/0 (monofilaments, braided, absorbable, etc.).
- Ultra-thin film of tetrafluoroethylene with a thickness of 25-40 microns.
- A set of instruments for operations on tendons (Rozova).
- A set of microinstruments for operations on small vessels and nerves up to 3 mm in diameter.
Surgeon Qualification
The best anatomical and functional results in the treatment of patients with severe hand injuries can only be achieved by a surgeon who specializes in hand surgery, has sufficient experience in such operations and is constantly aimed at improving skills, keeping up with the rapid progress of surgical technologies.
Such a specialist can be a traumatologist with good general surgical training, who has passed the appropriate specialization.
A specialist in the treatment of patients with severe hand injuries should consider the following:
a – damage mechanism;
b - zone and level of damage;
c - the nature of the wound (the degree of mechanical and microbial contamination);
d - profession and age of the patient;
e - the level of intellectual development of the victim.
The role of a specialist in hand surgery increases significantly when providing specialized medical care wounded in the hand, as well as when performing reconstructive operations in the long term. Such operations, in addition to skill, require non-standard thinking and the exertion of professional forces.
A specialist in hand surgery must master the technique of microsurgical manipulations, sometimes many hours, therefore certain requirements are imposed on health, diligence, dedication, constant training of professional skills.
Anesthesia
When performing surgical interventions on the hand general anesthesia rarely used. As experience shows, in 70% of cases anesthesia is provided by traumatologists themselves, using various methods of local and conduction anesthesia.
The traumatologist must master one of the methods of conduction anesthesia. Regardless of the method of anesthesia, it must meet the following requirements:
a) provide sufficient length and depth;
b) create an opportunity for the surgeon to contact the victim, i.e. do not turn off consciousness;
c) not cause general and local complications.
Primary surgical treatment of wounds of the hand (PHO) with
damage to tendons, neurovascular formations and
bones.
There are early (performed within 24 hours), delayed (up to 48 hours) and late (more than 48 hours) PST. As a rule, it is indicated for victims with open fractures, dislocations and bone defects, deep lacerated wounds and soft tissue defects, as well as for incomplete and complete detachment of fingers (hands).
Requirements for PST of hand wounds: atraumatic; marginal economy; reasonable radicalism; maximum preservation of the segment.
For a surgeon who has not specialized in hand surgery, tactics should be considered acceptable when, upon admission of the victim, he is limited to the toilet of the wound, stopping external bleeding, suturing (only on the incised wound) and immobilizing the segment. In this case, the patient should be referred to a specialized hospital. If this requirement is not met, the damaged tendons are displaced in their canals and fixed with scar tissue. Restoring function becomes problematic or impossible. The current level of development of hand surgery involves, along with PST, to perform the entire complex of reconstructive and restorative operations.
What should be done during the primary surgical treatment of wounds of the hand and fingers? First, the lacerated wound should be turned into a cut wound (the goal is the primary healing of the wound). Secondly, it is necessary to dissect the wound to conduct an exhaustive diagnosis of damage. Then it is required to restore all damaged structures (bones, tendons, blood vessels, nerves) and perform plastic surgery, if necessary.
These are the first steps. After wound healing, the main content of treatment is an individual program aimed at restoring the function of the hand lost as a result of injury. Primary surgical treatment, carried out by an experienced specialist, lays a solid foundation for effective restorative treatment.
Diagnostics
A variety of damaging factors, a high density of important anatomical formations, determine the complexity of diagnosis, surgical operations, rehabilitation.
The search for rational methods for restoring the function of damaged tendons has been going on for more than 100 years. An emotionally truthful assessment of the difficulty of restorative treatment of tendons belongs to A.M. Volkova (1991). "Perhaps in no other branch of surgery are there so many disappointments with unsatisfactory functional results as in flexor tendon surgery."
The high rate of unsatisfactory results is caused by the following factors:
Significant density and tightness of the walls of the bone-fibrous canals;
The complexity of the form of bone-fibrous canals;
Significant tendon mobility, providing the function of the fingers;
Inevitable, biologically natural formation of cicatricial adhesions of tendons in case of any damage.
Diagnosis of damage to the deep and superficial flexors of the fingers is not difficult (Fig. 2, 3).
Primary recovery of damaged finger flexor tendons is possible if a number of conditions are met:
- The victim must be hospitalized in a specialized medical institution, where reconstructive surgery and rehabilitation treatment can be performed.
- The medical institution must have the appropriate facilities and equipment (see above).
- The specialist of a medical institution must meet the requirements:
a) understand in detail the normal, variant and pathological anatomy of the hand;
b) know and be able to perform several options for each specific reconstructive and restoration operation;
c) observe the patient until the final outcome.
- The patient is obliged to strictly and accurately comply with all medical prescriptions. The success of treatment is possible only with the joint efforts of the doctor and the patient.
Operations for primary injuries of the flexor tendons of the fingers
Repair of an injured finger flexor tendon should not be delayed. If necessary, PST is carried out in order to create conditions for the primary tendon suture.
General rules for applying a tendon suture to the flexors of the fingers
Avoid longitudinal incisions on the fingers, which lead to additional damage to the supporting ligaments of the flexor tendons (Fig. 4).
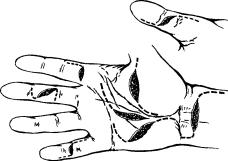
Scheme of skin incisions during operations on the flexor tendons.
- The proximal ends should be exposed through an additional transverse approach along the line of the distal palmar crease.
- Minimally injure the bone-fibrous canal; access to the area of the tendon suture to expand due to the "valve" flaps of the bone-fibrous canal, which are restored at the end of the operation.
- The seam should be made with a thin strong thread with the lowest coefficient of linear stretching (lavsan No. 4 and its analogues). Additional adaptation of the tendon edges with a thin absorbable suture is required (sutures of the Dexon type No. 6, PDS II No. 5.6, etc.).
- Tendon suture requirements:
a) the seam should be simple and easy to perform;
b) the ends of the sutured tendon must be matched without gathers, twists and deformations;
c) firmly fix the ends of the tendon, prevent cicatricial diastasis between the ends of the tendon;
d) preservation of the sliding surface of the tendon;
e) preservation of intra-stem circulation in the tendon and, if possible, in the paratenon;
e) the suture should not cause a reaction of the tendon tissue or its defibration;
g) the retaining suture is made with a non-removable thread with the knots immersed in the thickness of the tendon.
More than 70 types of tendon suture are known. Such a number does not indicate perfection, but that none of the seams proposed so far is without serious shortcomings.
The recommended type of suture is a spiral (spatially rotated) Kuneo suture. It meets all the requirements for a tendon suture. A relative disadvantage of this type of seam is the need for careful application of it. A carelessly performed Cuneo suture leads to rough scarring and fusion of the walls of the osteofibrous canal with the sutured ends of the tendon.
The choice of suture thread should be given the most serious attention. In recent years, a large amount of atraumatic suture material has appeared, including for tendon sutures. Among the most commonly used imported threads for applying a retaining suture, it is recommended: e tilon № 2/0, mersilk № 0, mersilene № 2.
Domestic suture material is more accessible, much cheaper, and with the right selection in terms of fixation strength, the absence of undesirable properties is not inferior to imported. These requirements are met braided lavsan No. 4. It is necessary to warn traumatologists against the use of domestic nylon suture material. It has a high coefficient of linear tension and cannot be used to connect the ends of damaged tendons.
Method of primary suture of deep flexor tendons
In case of tendon injuries, 5 zones are distinguished. At the level of each of them, the recovery technique has its own characteristics and differences, which have a significant impact on the final result.
Consider specific clinical examples.
Zone 1. Option 1. Initial data: incised wound in the transverse direction, with cutting off the tendon almost from the place of attachment to the nail phalanx.
Favorable variant of damage. Surgical intervention consists in the reinsertion of the tendon.
 |
 |
|
|
|
Fig.5 Scheme of reinsertion of the deep flexor tendon with a transosseous suture. |
Fig.6 Tendon fixation option a) paraossally; b) with reverse thread through the nail plate |
||
Methodology. The proximal end of the tendon is squeezed into the wound by bending the hand and fingers. If this technique fails, a transverse approach (1 cm) should be made at the level of the proximal interphalangeal joint. As a rule, the end of the tendon is located near this level, since it is kept from further displacement by a feeding structure - the mesentery, which emanates from the superficial flexor tendon.
The tendon is sutured in one of the following ways: according to Frisch, Rozov, Kuneo or Bennel, and the threads are carried out in the distal direction by means of a wire loop. Next, 1-2 channels are applied in the nail phalanx, through which the thread is brought out to the nail plate and tied with tension. Stitches on the skin. Bandage. Finger movements begin from 5 to 6 days. After 4-5 weeks. the button is cut off, the patient is recommended to develop movements with a load (balls, expanders).
Zone 1. Option 2. Initial data: incised wound in the transverse direction at the level of the middle phalanx. The length of the distal segment of the tendon is 0.5-1 cm.
 |
 |
 |
|
Fig.7 Scheme of the intra-stem suture of the tendon |
||
Methodology. In this case, the intra-stem suture method is the most justified (Fig. 7). It consists in the following: the central end of the damaged tendon is found and brought into the wound, then stitched along Kuneo, Frisch or Lange. The main thing is that when checking for strength, the seam does not slip and does not deform the tendon. Next, the tendon is passed into the canal, both threads are inserted into the peripheral segment with a straight tendon needle and brought out to the fingertip. Through the same puncture, they are transferred to the nail phalanx through a channel made with an awl. The thread is fixed on a button.
In some cases, fixation of the tendon to the nail phalanx by transosseous threading is not feasible or is not rational.
For this, a fixation method is proposed that does not involve the application of a channel in the nail phalanx. It consists in the following. With a bayonet-like access, the flexor tendon, torn from the nail phalanx, is exposed. Trying not to damage the sliding surfaces, the tendon is stitched along Frisch, Kuneo or Lange; after that, both free ends of the thread are loaded into a straight thick tendon needle. Having made a needle injection at the base of the nail phalanx parallel to the latter, the needle is passed under the nail matrix to the fingertip. By reverse injection, both threads are alternately passed to the surface of the nail phalanx, where they are fixed with an interrupted suture for 4 weeks (Fig. 5).
Zone 1. Option 3. Initial data: an incised wound in the area of the proximal interphalangeal joint, the length of the peripheral segment is more than 1 cm
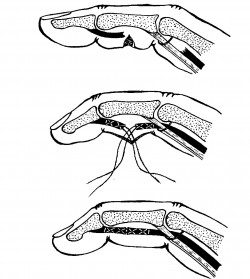
Fig.8 Scheme of the suture of the flexor tendon at the level of the middle phalanx
In this case, fixing the tendon to the nail phalanx is not possible. Threads passed through the peripheral segment of the tendon can cut through the tendon tissue and damage the walls of the bone-fibrous canal. The inevitable inflammation will intensify the scarring process. In this case, the wound is expanded to the sides, a revision is performed. In order to trace the integrity of the legs of the superficial flexor, nerves and terminal branches of the digital arteries. The tendon ends are stitched along Kuneo, brought together, in this position the threads are tied. The intramural suture is completed by applying a twisting adaptive suture according to Kleinert (scheme) with a 5/0-6/0 Supramid, Etylon or Dexon 4/0, Dexon II Plus thread (Fig. 9).

Fig.9 Scheme of a tendon suture according to Kuneo with an adaptive suture according to Kleinert.
Zone 2. The most difficult to restore tendons.
Synonyms: "no man's land", "no man's land", "no man's land", "damned zone", etc. The complexity is due to: the peculiarities of the anatomical structure, the large amplitude of the displacement of the deep tendon, the significant loads that fall on this level. The boundaries of the zone: the middle third of the middle phalanx - the proximal edge of the first annular ligament of the finger (diagram).
At this level, the thin-lamellar tendon half-tube (this is what the tendon of the superficial flexor looks like) divides into 2 legs, which are attached to the lateral parts of the middle phalanx. Through this half-tube passes a cylindrical tendon of the deep flexor. The anatomical ensemble is completed by an annular ligament, closely adjacent to both tendons.
Several types of damage occur at this level. The most typical of them.
Option 1 . The deep flexor was transected at a distance of 1.5 cm from the nail phalanx, the superficial one was preserved.
The solution here is as simple as the damage itself: an intra-bore submerged seam. In this case, the superficial flexor should not be excised.
Option 2. The deep flexor was damaged at a level of 1.5 cm from the point of attachment to the nail phalanx, the superficial pedicles were crossed (one or both).
Solution. Damage is classified as complex. In most cases, in such a situation, excision of the superficial flexor is resorted to, since it is believed that it interferes with excursions of the fused deep flexor tendon. But it's not.
The tendon of the superficial flexor accounts for 60% of the flexion force, so the role of its preservation is great. In this situation, they resort to the seam of the legs with the threads brought out to the side surfaces of the middle phalanx (Fig. 10), where they were fixed with buttons. In the vast majority of cases, the level of damage to the deep flexor tendon is displaced by 0.5-1.0 cm more in the central or peripheral directions (due to the position of the fingers at the time of injury). In this regard, after an intratruncal suture, the scarring process does not affect the tendon of the superficial flexor. Of course, thoughtful recommendations are needed throughout the entire period of rehabilitation, primarily on the motor regimen.
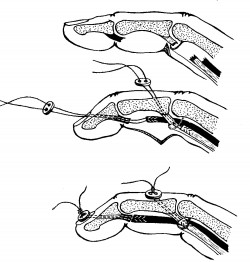
Fig.10 Reconstruction scheme for both flexor tendons
Option 3. Both flexors are damaged, and the superficial one is at the level of the tendon junction (chiazma tendinum), and the deep one is close to it.
Solution. The tendon of the superficial flexor is to be excised. This is a forced measure, but it must be resorted to, otherwise both tendons will fuse together, and the range of motion will determine the tendon of the superficial flexor (at best). At worst, there will be no movement. Clipping of the tendon of the superficial flexor should be performed from a small additional incision in the palm, which is carried out along one of the palmar folds (better - along the distal one). Together with the superficial, the deep flexor tendon is also brought into this wound, where it can be more easily stitched.
The peripheral segment is stitched either with a bent finger, when the tendon is, as it were, “born” from the bone-fibrous canal, or from an extended access (linear incision 1-2 cm along the palmar-lateral surface of the finger). At the next stage, using a wire guide, the central end of the deep flexor tendon is passed into the bone-fibrous canal to the level of damage, where it is sutured (Cuneo suture + twist suture). If necessary, restore the annular ligaments.
Similarly, the deep flexor tendon is restored at a more proximal level, including the annular ligament at the base of the finger. Since there are no rules without exceptions, there are also here. In some cases, the pedicles of the superficial flexor tendon start almost from the level of the base of the finger, which is a favorable condition for the restoration of both tendons (2 pedicles of the superficial and deep). For the seam of the legs with this option, a seam according to Lange, Frisch or Rozov is preferable.
Zone 3. Borders - the proximal edge of the annular ligament - the peripheral edge of the ligament of the wrist joint (carpal).
Zone features. The tendons are in close connection with the neurovascular bundles of the common digital nerves and common digital arteries. Superficial arterial arch. In the elderly, deviations in the anatomy of the 3rd zone of the hand are possible due to cicatricial changes in the palmar aponeurosis (Dupuytren's disease) or previous injuries, inflammatory diseases and so on.
Superficial location of the median nerve at the outlet of the carpal ligament. Quadratus morti at the base of the palm and 1 ray.
The zone is characterized by frequent damage to several tendons of 2 or more fingers at once. More frequent are concomitant damage to the nerves, arteries.
In practice, there are several options for damage to the flexor tendons in this area.
Option 1 . Isolated damage to the flexor tendons of one finger at the level of the central part of the palm.
Solution. An intra-stem suture is applied with a strong thread to each of the tendons.
IN postoperative period– early movements, late loading.
Option 2. Damage to 3-4 flexors on 2-3 fingers in the center of the palm.
Solution. Each of the tendons is subject to restoration by applying a strong intra-stem submersible suture based on an early dosed load. It is permissible to use adipose tissue, part of the wall of the bone-fibrous canal or tendon sheath as a lining between the tendons.
Option 3. Damage to 2-3 flexor tendons at the base of the palm.
Solution. All tendons are subject to restoration through the imposition of a strong intra-stem submersible suture. In the case of suturing the superficial and deep flexors at the same time, it is highly desirable to use the short muscles of the palm (worm-shaped) as a gasket. To do this, the muscle is moved with minimal trauma under the superficial flexor and fixed with 2-3 absorbable sutures. In this case, it becomes possible to achieve the maximum result in the form of a complete restoration of the function of the fingers.
Zone 4. The boundaries of the zone practically depend on the width of the carpal ligament + 0.5-1 cm proximal and distal to it.
Zone features. The tendons are in contact with a tight bundle in the walls of the canal. Together with the trunk of the median nerve, outwardly no different from the tendons. Numerous examples of erroneous stitching of the ends of the nerve with the ends of certain tendons are associated with this.
Tendon injuries at this level are fortunately rare. The restoration of tendons damaged as a result of an injury here practically does not differ in technique from their restoration in zone 3. A feature of the planning of the operation is the mandatory resection of the carpal ligament along its entire length, since the fused tendons inevitably increase in diameter and can block the function of all other tendons that run in close proximity to the sutured tendon by cicatricial adhesions. It is impossible to be limited only to dissection of the ligament. In this case, the newly formed scars will form a narrower channel than before the injury, increasing the pressure on the tendon, like a noose. As a result, dysfunction of all tendons is possible.
Zone 5. Borders: the proximal edge of the carpal ligament is the transition of the tendons to the muscular bellies. The flexor tendons of the fingers complement the flexor tendons of the hand itself. In addition, the main arteries pass - the radial and ulnar, as well as the ulnar and median nerves with their accompanying veins.
Zone features:
1) the presence of the Pirogov space;
2) the presence of main arteries, veins and nerve trunks of a relatively large section;
3) the absence of tendon sheaths and bone-fibrous canals.
The features noted above significantly affect both the nature of the injuries and their severity, and the approach to the restoration of damaged tendons.
Thus, ulnar injuries of the lower third of the forearm, along with damage to the tendons, are often accompanied by the intersection of the ulnar neurovascular bundle. In the light of modern ideas, all elements need to be restored. In this case, the problem with the tendons is solved more easily by applying any of the many intra-stem sutures. Restoration of the vessel and nerve requires special skills and abilities from a traumatologist.
If damage to several tendons occurs at the level of zone 5, the problem is also not difficult - intra-trunk sutures are applied to the ends of the tendons. It is difficult to identify tendons of the same name.
There are tricks by which this can be done. So, at the entrance to the flexor canal, the tendons of the superficial and deep flexors are arranged in a certain order, knowing which, it is possible to identify the ends of the tendons.
One of the landmarks may be the typical location of the ulnar artery with the nerve (only the tendon of the ulnar flexor of the hand passes below them), the radial artery (above it is the passage of the radial flexor of the hand and the tendon of the long flexor of the 1st finger). Thus, 8 tendons of II-V fingers remain. But here, too, there are some guidelines. As a rule, with expanded access to damaged flexor tendons in the lower third of the forearm, it is possible to divide all tendons into two groups - superficial and deep flexors. It is somewhat more difficult to do this in brachycephalic subjects, i.e. squat people, with short thick arms, it is easier - in dolichocephals.
The division into groups is carried out on the basis of the following features: the muscles of the tendons of the superficial flexors are located immediately under their own fascia of the forearm, and deep - under them; the bottom of the deep is the interosseous membrane (Pirogov's space).
The next stage of identification is the determination of the flexor tendons of the fifth finger (we consider the case of complete intersection of all structures of the volar surface of the forearm to the interosseous membrane). Landmarks: these tendons are thinner, so much so that they differ from the rest, located immediately above the ulnar neurovascular bundle closer to the midline of the forearm.
The flexor tendons of the II-III-IV fingers remain. Again, their location will help identify the tendons of the second finger - they go next to the radial artery, a little closer to the midline of the forearm than the radial artery. These tendons should not be confused with the tendon of the long flexor of the 1st finger. This should be dealt with separately. The tendon of the long flexor of the 1st finger, despite its name, has a shorter tendon part: after leaving the flexor canal, it goes deepest and obliquely, having a general direction towards the lower third of the ulna. In addition, the muscular belly in some cases begins at a distance of 3-4 cm of the carpal ligament and serves as an excellent guide for identification. It should not be confused with the transverse fibers of the quadrate pronator of the hand.
As for the tendons of the III-IV fingers, some identification nuances can be recommended for practical surgeons for them.
So, the superficial flexors of the IV and V fingers often fuse together and go as a single lamellar cord. The same picture is often characteristic of the tendons of the deep flexors of the IV and V fingers. The distinctive features of the superficial and deep flexor tendons have already been discussed. The flexor tendons of the third finger remain. If there are no other benchmarks, then they are determined by the residual principle. In other cases, the proximity of the superficial flexor tendons to the median nerve may provide some assistance. It is necessary to be careful not to allow the seam of one of the ends of the nerve with the tendon of the third finger. With the help of an operating magnifier, it is possible to examine the details inherent only to the nerve: small convoluted vessels on the surface, an intrastem artery on the cut, which bleeds if a blood clot is removed from the lumen of the artery with a wet swab dipped in a heparin solution. In addition, the nerve has a more pronounced shady pattern, less shiny than the tendon, especially in young people. In addition, with light traction for the central segment of the nerve, the muscles do not move, for the peripheral one - the fingers, primarily III, do not bend. It is possible to simplify the identification of the peripheral ends of the flexor tendons by simply traction on the corresponding tendon. All of the above applies to a greater extent, of course, to the central ends of the tendons. The verification of the correctness of identification is the exact match of the tendon sections after the intratruncal suture is applied. Of course, we are talking, first of all, about such injuries as cut wounds.
Restoration of tendons, nerves, arteries of the forearm is a laborious and lengthy procedure. Some specialists allow themselves to separately restore only the tendons of the deep flexors, and the superficial ones are sewn together as a single block. This technique of repair should be strongly objected to and seeks selective tendon repair. In other words, each tendon is subject to suturing separately, despite the threat of scarring of all sutured tendons into a single block. To prevent such an outcome in the rehabilitation period, separate movements are recommended with each finger individually, starting from 4-5 days after the operation. With this approach, the severity of scars is less, they do not block adjacent tendons, and in the long term, the results exceed all expectations.
Due to the large number of damaged structures, the question of the order of restoration arises.
Naturally, in case of arterial blood flow decompensation, the artery is sutured first. The choice in favor of the restoration of one or another artery is decided simply: they restore more large artery. This is usually radial, but it also happens vice versa. At the same time, the surgeon, having restored the artery, complicates the process of restoring the tendon of the long flexor of the 1st finger. It is located under the artery, if we consider the level 4-5 cm above the carpal ligament. Thus, it is advisable to suture this tendon in the first turn, and then proceed to the restoration of the artery. The tendon suture of one tendon does not take much time, so transcendental ischemia cannot occur. This tactic is more preferable, since the surgeon does not injure the artery and its thrombosis does not occur.
The second stage restores the remaining tendons of the deep group. The recovery sequence is not critical. The main thing is to prevent overstretching of any of the tendons, which can adversely affect the position of the fingers in the long term: one or another finger will either sag, or, conversely, have extension limitation. This is less important for the tendons of the superficial flexors, but here, too, the thoroughness of the tendon suture is decisive for the success of the operation as a whole.
To successfully restore the sliding of all tendons, it is advisable to use spacers between the group of superficial and deep tendons, and, in some cases, in the Pirogov space. The most suitable material is a 25-40 µm ultrathin film of tetrafluoroethylene. Placed between the tendons and fixed with a sufficient number of separate sutures, it is an excellent insulator. It does not require removal, is well tolerated by patients, and contributes to the formation of optimal scars at the site of tendon injury. From other materials, cutting out the fascia from the superficial flexors can be recommended. It is possible to cut out a sheet 3-3.5 cm wide and up to 8-10 cm long. This is usually enough to isolate the tendons. The disadvantage of this material is its cicatricial fusion with stitched tendons; this reduces the value of the fascia as a tendon insulator. It is also possible to use individual muscles as insulators, for example, a square pronator.
Two-stage tendon plasty.
At the first stage, by carefully dissecting the scars with the vessels and nerves of the fingers sealed in them, a canal is formed. A Teflon rod or tube is placed in it. At the same stage, soft tissue structures - nerves, vessels, annular ligaments - can be restored. In the second stage, 8 weeks later, with an uncomplicated course of the reparation process, the rod is replaced with a tendon autograft. The newly formed walls of the canal during microscopic examination during this period most correspond to the requirements for the tendon sheath. The best way to fix the tendon graft to the nail phalanx, from our point of view, is the method of Bennel (1942). At the level of the forearm, the tendon is woven into the tendon stump and stitched with separate interrupted sutures (Pulvertaft method). The second stage solves the problem - restoring the continuity of the tendon, which is also not the main thing in the treatment. Restorative treatment of the patient is of decisive importance.
Early movement of the tendons in the bone-fibrous canal is the simplest and most easily accessible way to prevent the formation of strong cicatricial adhesions in the postoperative period. Many experts use early active movements, considering this path to be the only correct one. But movements can also have an undesirable effect in the form of activation of fibroplastic processes (Mason M.L., Allen M.E.). With a constant and intense load, active movements by the end of the third week, when powerful scars develop, become impossible.
Technique for developing active finger movements in the postoperative period.
It should combine the advantages of rest and the dignity of movement and be as follows. During the first 3-4 days, rest of the operated limb is provided. After the edema has subsided, the tendon is moved to its fullest possible amplitude by actively flexing the finger(s). Single movements of the tendon do not cause an active alternative-exudative reaction from the walls of the tendon sheath. A day later, the tendon is moved in the opposite direction, also in an active way. Both positions are fixed with removable plaster splints. The technique is aimed not at breaking the adhesions formed between the canal wall and the tendon, but at stretching them. By the end of the third week, most patients manage to obtain a satisfactory amplitude of finger flexion. Further development of movements is carried out using expanders (foam, rubber, spring, etc.). The final result is taken into account no earlier than 6-7 months. after operation. Sometimes the progress of increasing the amplitude of movements lasts up to 8-12 months. It should be noted that the character of the patient, his perseverance and perseverance are of great importance in achieving success. This technique can be supplemented with physiotherapy treatment. However, we did not notice a significant difference in the results.
REHABILITATION
This is a complex, lengthy and painstaking work with each patient, one might even say that with each finger of each patient. It requires patience from both the patient and the doctor. Rehabilitation is carried out by a rehabilitation doctor, but the responsibility for final result still lies with the operating surgeon. The duration of rehabilitation can be different - from several weeks to several months. All this time, the patient should not be discharged for work, otherwise all efforts will go to waste. Industrial activity and work are incompatible.
Unlike tendon injuries flexor tendon injuries are often neglected, which is associated with the widespread idea of relatively favorable outcomes in injuries of this localization, with a low incidence of late complications. Nevertheless, the extensor tendons represent the final structure of a complex apparatus that ensures the transmission of the efforts of the external and internal muscles of the balanced function of the finger necessary for a person (“external” refers to the muscles that are represented only by their tendons on the hand). Damage at any level of this well-functioning mechanism, whether it be bone, skin, tendon-muscle formations, vessels or nerves, can lead to stiffness and disorganization of the functions of the fingers.
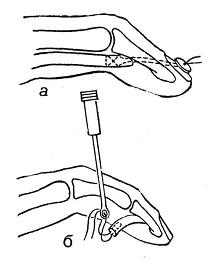
For ease of evaluation damage, and to a certain extent for the choice of treatment method, the extensor tendon in the area of the hand and distal the forearms are divided into eight zones. Damage to zone I (hammer toe) is accompanied by a violation of the extension mechanism at the level of the distal interphalangeal joint, resulting in a typical hammer toe deformity. This closed injury is the result of a sudden flexion of the terminal phalanx, which is in the position of maximum extension. As a result, there is a rupture of the end of the tendon or a detachment of the tendon from the bone along with bone fragments of various sizes. Active extension of the distal phalanx becomes impossible. A similar deformity may be the result of incised wounds or other open injuries of the skin, combined with a tendon injury.
IN early dates treatment of closed tendon injuries at the level of the distal interphalangeal joint should consist of splinting for up to six weeks in the extension position of the terminal phalanx. Other joints of the finger or hand must remain unblocked, including the need to maintain active movement in the proximal interphalangeal joints. If, at the end of the 6-week period, extension is difficult, it is possible to continue immobilization only at night for the next six weeks, followed by strict control. For any recurrence, continuous splinting should be resumed for another three weeks. With prolonged use of plaster immobilization, it is necessary to pay attention to the condition of the skin in order to avoid their maceration and necrosis. For more reliable assistance with subluxation in the distal interphalangeal joints, one of the methods of surgical fixation with knitting needles is sometimes used.
open damage mallet finger type can be a serious medical problem. With transverse cut wounds the tendon and skin are best sutured with separate sutures using non-absorbable sutures. If the ends cannot be brought together, they resort to skin grafting and primary plastic replacement of the tendon defect, or reconstructive surgery in a later period. Emergency care includes lavage of the wound/joint, dressing, application of broad-spectrum antibiotics, splinting in the extension position, and subsequent rapid preparation for surgery, which should take place within the next 24 hours.
Zone II includes tendon injuries in the projection of the diaphysis of the middle phalanx. The cause of the injury is usually associated with incised wounds or open fractures. Tendon injury less than 50% of its width without loss of extension function can be treated conservatively, with wound care and 7-10 days of splinting in the extension position, followed by active movement development. If more than 50% damage or DMFS extension is difficult, tendon continuity should be restored, followed by splinting or fixation of the extended DMFS with knitting needles for 6-8 weeks according to the hammer toe treatment protocol. In case of open fractures with an injury to the extensor, the fracture is treated and the tendon is reconstructed, followed by a set of measures aimed at restoring motor activity.
Separation central leg Tendon sprain in the area of its attachment to the middle phalanx is classified as a zone III injury with an initial violation of the extension mechanism in the PMFS. In the absence of treatment, such injuries end in subluxation of the lateral portions of the extensor in the palmar direction, with the development, after 1-2 weeks, of a classic boutonniere-type deformity, in which the middle phalanx is bent and the end is in the hyperextension position. Examination of the patient reveals limited or no active extension in the PMFS. With closed fresh injury pain and swelling in the PMPS area can make it difficult to diagnose a detachment of the central pedicle. In such cases, the most rational tactics include splinting the extended PMFS, monitoring the patient and re-examination after seven days. Metacarpophalangeal and DMFS are not subject to immobilization together with PMFS. If after a week the diagnosis of a closed central pedicle avulsion is confirmed clinical manifestations, plaster immobilization is continued for 4-6 weeks with a weekly inspection. At the end of the immobilization period, planned rehabilitation of the full range of motion follows.
At open damage zone III perform wound treatment, including washing, removal of non-viable tissues, arthrotomy according to indications and plastic closure of the defect with a lack of local soft tissues. The tendon is repaired with primary sutures or allowed to heal naturally under transarticular pin fixation for 4-6 weeks. In this zone, there is a possibility of healing by secondary intention, since due to the structure of the extensor apparatus, retraction of the detached part does not occur while the PMFS is held in the extensor position.
Zone IV located above the proximal phalanx. Injury to the extensor tendon in this area is often the result of a fracture of the proximal phalanx. The tendon sprain here is quite wide, which explains the high frequency of incomplete ruptures. But even with a complete rupture, the detached tendon does not migrate proximally, but is held in place by sagittal bundles, similar to zone III injuries.
Tendon sprain at the level of zone IV affects a relatively wide space, therefore, in most cases, for the completeness of the examination and treatment, it becomes necessary to expand the incised wounds surgically. In some patients, it is possible to bring the ends of the tendon closer together with intratendinous sutures. But since the tendon bundle in this area often remains flat, this type of suture may not hold the connection in a reliable state. In such cases, the tendon can be sutured with simple single or "near/far-far/near" sutures (horizontal mattress sutures) to accomplish the task. Early movements in active flexion and passive extension are recommended.
If zone IV damage combined with fractures of the proximal phalanx, then stable fixation of the fracture greatly simplifies the early connection of the tendon to the work of the finger.
Zone V open injuries usually arise from a punch to the opponent's teeth. In this chapter, the treatment of such wounds is discussed in the section "Infection". Closed injuries are not typical for this area and, as a rule, affect the radial portion of the transverse ligament, which leads to subluxation or dislocation of the extensor tendon of the fingers into the intermetacarpal space on the ulnar side. It should be remembered that such an injury can occur in older people against the background of involutive changes.

If you can deliver diagnosis in the next 2-3 weeks after injury, then a traumatic or degenerative transverse ligament tear can be treated conservatively. To do this, the joints are fixed with a plaster cast, in which the wrist is in a neutral position, the metacarpophalangeal PPS (MPJ) are extended, and the PMPS and DMPS are free, or a bridge splint specially designed for damage to the transverse ligament is applied in the same position of the finger. In case of late diagnosis or unsatisfactory results of 6-8 weeks of splinting, tendon centering should be performed operatively.
Zone VI damage localized distal or proximal to the tendon joints that connect the tendons of the common extensor (CER). It is not always easy to detect proximally located damage to one tendon of the RRP, since the extension of the finger in the PFS is not affected by the indirect action of the adjacent tendon through the tendon junction. Additional Methods examinations, such as ultrasound or MRI, are of low diagnostic value in such a situation, and the only way to make a diagnosis is a physical examination. Similarly, the diagnosis of ruptures of the extensors of the index finger (IF) and the smallest finger (RN) is difficult, since their extension can provide ORP. Both a rupture of the RJ proximal to the tendon junction and an isolated injury to the RJ or RJ tendon will result in displacement of the proximal end of the tendon. Often, the end of the tendon of the RUP or RNP can go to the level of the extensor retinaculum. In this regard, examination in the operating room is more appropriate than in the department. emergency care. As a rule, tendon injury at this level can be repaired with intratruncal sutures, supplemented by suturing the epitendinium.
open zone VI damage can be combined with extensive soft tissue defects, which often requires staged skin grafting and primary or delayed restoration of the integrity of the tendon by suturing or by transplanting a tendon graft.
IN zone VII ruptures occur at the level of the tendon retinaculum, where the tendons of the muscles are located in six synovial sheaths. Damage to this area is also characterized by a displacement of the ends of the extensor, which makes the planned surgical intervention inevitable. Surgical treatment should be especially careful to avoid fusion of the tendon with the superior retainer, the lengthening of which often necessitates closing the wound with a Z-plasty. Retainer failure leads to pathological protrusion of the extensor tendons in the wrist area. Tendon ruptures can be combined with trauma to the sensory branches of the radial and ulnar nerves, damage to which should be remembered for rapid recognition and suturing of the nerves using microsurgical techniques. Left unattended, concomitant nerve injuries lead not only to loss of sensation in the area of the dorsum of the hand, but also to neuropathy with chronic pain syndrome.
Zone VIII damage touch the area of the extensor tendon-muscle junction. The injury here is always penetrating, with a small entry hole or massive soft tissue damage, and is often the result of open fractures of the bones of the forearm. On initial examination of a penetrating wound, usually a stab wound or a glass splinter cut, a discrepancy can be found between a relatively small skin wound and significant destruction of the underlying tissues, even with normal extension function preserved. As for the stitching of the tendon-muscle junction itself, the difficulty lies in eruption muscle tissue when tightening knots. Continuity of the connection is secured with big-eight sutures, followed by a period of immobilization for a period of four to six weeks at 20° wrist extension and 20° MFC flexion. good recovery functions is possible when the injury is localized distal to the posterior interosseous nerve of the forearm.
They account for 1.9 to 18.8% of all hand injuries. However, their value is determined not by the number, but by the severe consequences of the injury.
Tendon injuries are observed both with small stab, incised, chopped wounds, and with severe injuries of the hand. Tendon injury during trauma occurs in the wound, but depending on the position of the finger (flexed or extended), the cutting object, the position of the hand and muscle tension, it can shift.
By adhering to a certain examination technique, it is not difficult to recognize damage to the tendon, since the movement disorders associated with it are easily detected. As experience accumulates, the surgeon makes the correct diagnosis based on the location of the wound and the circumstances of the injury. For the purpose of diagnosis, one should not make unnecessary movements, look for the ends of the cut tendon in the wound without preparing the appropriate conditions for intervention on the tendon. Increased flexion attempts contribute to bleeding, rupture of the mesotenoneal ligaments, and divergence of the ends of the tendons.
Principles of treatment of tendon injuries. The tactics, technique and details of surgical interventions for injuries of the tendons of the hand have their own characteristics; they do not cease to be improved and discussed on the pages of the periodical press in almost all countries of the world. A huge literature is dedicated to them. It is now generally accepted that the difficulties of recovery and the results of the operation are different for injuries of the extensor and flexor tendons of the fingers. In addition, outcomes vary depending on the level of tendon injury. Surgeons also agree that the operation to restore the continuity of the flexor tendons, in the area of the synovial sheaths on the fingers and on the wrist, is a difficult intervention that requires special training of the surgeon and a special environment.
By the time of intervention, they now distinguish: primary suture - within 20 hours from the moment of injury, delayed - in the next 10-20 days after injury, subject to primary healing of an accidental wound. Tendoplasty is also divided into early - 20-30 days after the injury - and late, carried out in the long term (V.I. Rozov, 1952).
Primary surgical interventions on the tendons are not indicated: with contaminated incised wounds; with lacerated, bruised, crushed wounds, with multiple dislocations and fractures, even with proper surgical treatment and the use of antibiotics; in all those cases when the surgeon does not consider it possible to sew up the wound. Tendon surgeries are also not performed if there is no clean operating room, a fresh (not more than a day old) sterilized and unopened bix with surgical linen and dressings, appropriate instruments, an operating nurse, an assistant and a surgeon who knows the technique of tendon and nerve suture, and if it is not possible to observe the patient after the operation.
Primary suture of the flexor tendons of the fingers
Skin treatment is normal, exsanguination on the shoulder or forearm. With single injuries of the tendons on the forearm, when finding the ends and restoring lost relationships is not difficult, the primary suture of the tendon can be performed under local regional, intraosseous or intravenous anesthesia. In case of damage to the flexor tendons in the area of the wrist, palm and fingers, and in case of wounds complicated by dislocations and fractures, it is necessary to operate under anesthesia in a specialized hospital. Surgeons who have specialized in this field are guided by anesthesia, each with their own skill.
Wound treatment is performed according to the previously described method. Atraumatic intervention is achieved by the fact that the surgeon and the assistant do not unnecessarily touch, do not move, do not injure the tissues.
Of great importance are the sharpness and conformity of the instrumentation, suture material, sparing of the ligaments of the tendon sheath, careful attitude to tissues, moisturizing them during surgery, etc.
After excision of the wound, in order to expose the ends of the tendon, it is sometimes necessary to expand it to the sides, forming patchwork, or to make additional incisions along the projection of the course of the tendon. The greatest divergence of the ends is observed when the flexor tendons are injured in the area of the tendon sheaths and along the carpal tunnel. In order not to injure soft tissues with hooks, the edges of the wound are moved apart with a retractor or stitched with silk, moved apart or sutured to the skin away from the wound. The damaged ends of the tendon should not be grasped with coarse tweezers, they should be held with special clamps or stitched with a thin thread and taken to the "holders".
When the ends of the tendon are not mashed, they can not be excised, but limited to careful and gentle rubbing with a gauze ball moistened with furatsilin; mashed and bruised ends of the tendon are economically cut off with a razor. For a tendon suture, atraumatic needles, monolithic with a thread, are the best.
In the absence of them - a synthetic monolithic thread and other atraumatic suture materials and needles.
Taking into account the difference in the ratios of the flexor tendons of the fingers with the surrounding tissues, modern surgeons distinguish several zones and, in accordance with this, set indications for surgery in each specific zone.
When restoring the flexor tendons along the tendon sheaths, a hanging suture is used with a wire brought out according to the Bennel method, and its modifications. Indications for a particular method of tendon suture are determined by the localization of the tendon injury and the experience of the specialist surgeon.
The primary suture of the tendons of the flexors of the fingers in the area of the tendon sheaths in case of combined injuries of the tendons, bones and joints is possible only in the hands of a highly qualified specialist and under the appropriate conditions.
Rice. 121. Intra-stem sutures of tendons.
a - according to Cuneo; b - according to Bennel; c - according to Kazakov; g - according to Rozov; 9 - scheme of fastening the seams on the skin with a removable dry seam
In case of accidental damage to the tendon devices and their restoration, the tension of the tissues, which makes it difficult to slide, is unacceptable, so sometimes they have to be replaced with parathenon or fascia taken from the forearm.
Injuries to the flexor tendons at the level of the radiocarpal joint - in the area of the carpal tunnel - deserve special attention. The flexor tendons of the II-V fingers passing in it, protected by the ulnar synovial bag, are arranged in two rows, closely adjacent to each other. More deeply lie the tendons of the deep flexor and the tendon of the superficial flexor of the second finger.
The surface layer is formed by the tendons of the superficial flexor of the III-IV and V fingers, the median nerve and the tendon of the long flexor of the thumb (see Fig. 62). Directly at the pisiform bone, the ulnar artery and nerve pass through the ulnar canal of the wrist from the forearm to the palm.
With injuries to the palmar surface of the wrist, damage to the flexor tendons is often multiple and is combined with a wound to the median, less often to the ulnar nerve. Surgical care in the hospital should be provided by an experienced surgeon, as soon as possible after the injury.
Carpal tunnel tendon injuries are recognized by location, type of injury, mechanism of injury, and position and function of the fingers.
Treatment of tendon injuries at the level of the carpal tunnel is the primary surgical treatment of the wound, finding and connecting the central and peripheral ends of the damaged flexor tendons and nerves of the fingers. This operation requires a lot of time, proper conditions, environment, anesthetist, assistant and specialist surgeon.
It is recommended, having ensured proper access and cleanliness of the wound, to first revise the nerve trunks, guided by topographic and anatomical relationships. The matte color of the nerve, the presence of accompanying vessels nearby, the granular structure, and bleeding of the cut distinguish the nerve from the tendon. Finding the ends of the damaged tendons, it is advisable to start with the radial flexor of the hand, gradually squeeze out and bring into the wound and take all the proximal ends on the holders, and then, bending the fingers and hand, look for the distal ends. Only after the discovery of all damaged tendons and nerves, the integrity of the tendons is restored first, then the nerves. The practical implementation of this operation is very difficult, serious errors are not uncommon, and the results are often unsatisfactory.
In the presence of a clean wound without crushing the edges, it is possible to apply primary sutures to damaged tendons and nerves. After the suture of the tendon at the level of the carpal tunnel, adhesions often occur that impede the function of the tendons. To avoid this, some surgeons only suture the deep flexor tendons, partially excising the superficial flexor tendons.
A. M. Volkova (1975), based on the experience of treating combined injuries of the flexor tendons and nerves at the level of the carpal tunnel, reports the following results: complete recovery of functions was obtained in 45.8% of the victims, a good outcome - in 38.6%, satisfactory - in 15.6%. The author recommends the simultaneous restoration of tendons and nerves in a specialized hospital.
So, victims with injuries of the tendons in the area of the wrist joint should be immediately taken to a specialized surgical department for the operation of the primary or delayed suture of the flexor tendons and nerves of the hand.
Further treatment should be carried out by the surgeon who operated on the patient. With the persistent desire of the patient and patience, a satisfactory outcome can be achieved.
Features and imposition of the primary suture on the tendon of the long flexor of the thumb. The tendon of the long flexor of the thumb passes on the hand in the thickness of the muscles. It is enclosed throughout the synovial sheath, which is looser than the sheaths of the remaining fingers.
When the tendon of the long flexor of the thumb is damaged at the level of the metacarpophalangeal joint, it is difficult to find the central end in the thickness of the thenar muscles and often a significant expansion of the wound or an additional incision is required. It is also difficult to guide the tendon through the fibrous canal at the level of the metacarpophalangeal joint. In addition, when operating in this area, it is always necessary to anticipate the risk of damage to the sensory and motor branches of the median nerve (see Fig. 27).

Rice. 122. "Critical zone" for the suture of the flexor tendons of the fingers (shaded).

Rice. 123. Diagram of the transfixation technique for suture of the flexor tendons.
a - according to Pugachev; b - according to Verdan; c, d, e - according to Bstekh.
Nevertheless, the results of the suture and plasty of the tendon of the long flexor of the thumb are better than on adjacent fingers.
Primary suture of the flexor tendons on the palm
Here, the flexor tendons of the II-III-IV fingers, surrounded by a loose peritendinium for 1.5-2 cm, pass outside the synovial sheaths. The results of their recovery are more favorable. Injuries to the flexor tendons in this area are often multiple and complicated by injury to the digital nerves.
The suture of the tendons of the flexors of the fingers in the area of the synovial sheaths in the "critical zone" is difficult and gives worse results (Fig. 122). The issue of primary, delayed suture and tendoplasty of the flexors in the area of the tendon sheaths in practice, each surgeon has the right to decide according to his experience and specific conditions.
According to the opinion of most modern surgeons, the primary suture of the tendon along the “critical zone” can only be used under ideal conditions: a clean wound with smooth edges without complications of bone damage and without a defect in the skin and no later than 6 hours from the moment of injury.
Rice. 124. Scheme of transosseous fixation of the central (a) and peripheral end (b) of the deep flexor tendon.
The principal setting is briefly reduced to the following. When tendons are injured in the “critical zone”, only the deep flexor of the fingers is restored. The central end of the superficial flexor tendon is sutured to the deep, proximal to the tendon suture, outside the tendon sheath. This detail not only helps to maintain the strength of the finger, but also maintains muscle balance. Most surgeons (N. M. Vodyanov, 1973; Bsteh, 1956; Verdan, 1960) use a transfixation technique with “supporting” sutures to suture the flexor tendons in the area of the tendon sheaths (Fig. 123).
With this method, after excision of the wound, the area of damage to the tendon sheath expands in the proximal and distal directions, but, as far as possible, the retaining annular and cruciate ligaments are preserved. If the central end of the tendon is not found in the wound, then an additional incision is made in the palm of the hand, from which it is brought into the wound to the distal end. In the area of the palmar wound, under the control of the eye, the central end of the deep flexor through the skin, the palmar aponeurosis and the superficial flexor is pierced with a stainless needle and fixed to the periosteum of the metacarpal bone in the corresponding interosseous space.
The tension force of the muscles with this method is removed, and the adjacent ends of the tendon on the finger can not be sutured or only adaptive sutures can be applied to the peritenonium, then the ligamentous apparatus of the tendon sheath is restored according to the method of S. I. Degtyareva (1970) or in another way. To avoid adhesions, it is recommended to partially excise the tendon sheath at the level of damage within 0.5-1 cm. The operation ends with careful hemostasis and a blind suture of the wound; immobilization of the hand with a modeled back plaster splint. The duration of immobilization depends on the period of tendon regeneration and on the consolidation of the fracture in case of associated injuries. The needles fixing the tendon are removed after 3 weeks. In case of damage to the deep flexor tendon at the level of the distal interphalangeal joint, fixation of the central end to the distal phalanx with a transosseous removable suture is shown (V. S. Dedushkin, 1976; Fig. 124).
Postoperative management of patients with damage to the tendons of the hand is very responsible. Special works are devoted to this issue (N. V. Kornilov et al., 1975, etc.). Of course, it is necessary to carry out postoperative treatment under the direct supervision of the operating surgeon together with the doctor of therapeutic exercises and a physiotherapist according to a developed, but always individualized scheme. Active movements are allowed only after removing the fixing needles and blocking threads - not earlier than 3 weeks. Active movements in the distal interphalangeal joints are carried out with saving fixation of the middle phalanx (V. I. Rozov, 1952). On average, after 1 1/2 - 2 months, patients are discharged to work.
Removable, facilitating or suspension sutures disrupt blood circulation to a lesser extent and are simpler than intramural ones, therefore several of their variants have already been developed and the improvement of details continues both here and abroad.
The conditions of an emergency intervention are always less favorable than a planned operation by a qualified surgeon in a calm environment. Therefore, the indications for a primary suture within the synovial-aponeurotic zone narrow in favor of a delayed suture and early tendoplasty.
The suture of the tendon of the deep flexor of the fingers at the level of the middle phalanx
In the transverse direction of the wound, often only the deep flexor tendon is damaged; the impossibility of bending the distal phalanx is found. Some surgeons recommend not suturing the tendon in such cases, but this leads to loss of the sculpted and other types of capture.
It is more correct to adhere to the tactics recommended back in 1952 by V.I. Rozov. If both ends of the deep flexor tendon are found in the wound during surgical treatment, then they are sutured in accordance with all the rules. When it is technically impossible to perform this suture, it is advisable to fix the proximal end to the distal phalanx with a transosseous removable suture. If only the peripheral end of the tendon is found, then tenodesis or arthrodesis of the joint is performed to provide support for the phalanx. Only in persons of "fine" professions is a reconstructive operation undertaken.
There is no consensus on the tactics of the surgeon in case of simultaneous damage to the flexor tendons of many fingers. Some recommend simultaneous repair of the tendons of only some of the most functionally important fingers, others prefer the simultaneous suturing of all tendons, and some prefer delayed tendon suture or early tendoplasty.
In 1956, the results of V. I. Rozov with the primary suture of 189 tendons of the flexors of the hand and fingers in 127 patients (according to a five-point assessment) were as follows: "5" - 26.4%; "4" - 27%, "3" 18.5 o / o, "2" 19%, "1" 2.2%, unknown 6.9%. We know the long-term results of the primary suture in 22 patients (30 sutured tendons): a good result was observed with 17 sutures, satisfactory - in 9, poor - with 4 tendon sutures.
O. V. Vladimirtsev (1972) notes a significant improvement in outcomes after the primary suture of the flexor tendons using an unloading nylon suture - up to 89.8% good, 6.8% satisfactory and 3.4% poor. Verdan (1972), reviewing a number of advances, notes the advantages of a primary suture in the hands of a specialist.
N. M. Vodyanov (1973), who has considerable experience, believes that with isolated injuries of the deep flexor tendon of the finger, a supporting primary suture is indicated up to 24 hours from the moment of injury to all victims, regardless of the nature of the injury, age and profession. He gives the following information about the results of the primary suture of the tendon of the deep flexor of the fingers in 75 patients: a good result - 53; satisfactory - 17, unsatisfactory - 5.
The optimal period for free plasty of the flexor tendons of the fingers is considered to be the first 2 months after injury, until degeneration of the distal segment of the injured tendon occurs. This reconstructive operation should be performed by specialists in hand surgery (S. I. Degtyareva, 1970; N. P. Demichev, 1977).
Restoration of the extensor tendons of the fingers, if there are no contraindications, is performed during the primary treatment of uncomplicated and complicated wounds of the fingers and hand.
The primary suture of the extensor tendons in case of single injuries can be performed on an outpatient basis in a trauma center if appropriate conditions are present. Secondary suture and tendoplasty are performed in a hospital.
Injuries to the extensor tendons are most often (59.5%) observed on the fingers, less often (34.6%) - in the metacarpal region, and only with extensive wounds their integrity is disturbed at the level of the wrist (5.9%).
Restoration of the extensor tendons during primary treatment does not present any special difficulties when the wound is inflicted with a sharp-cutting object. The distal and distal ends of the tendon are not far apart and are found in the wound or nearby tissues. The operation is performed in the following sequence: economical excision of the wound, restoration of disturbed relationships of the skeleton, joints, extensor tendon suture, nerve suture and wound closure. The extensor tendon can be connected with any suture, but it is preferable to apply a supporting or intratendinous suture that does not prevent slipping.
The secondary suture of the tendon is also made after the wound has healed, on the 8-10th day or later - after 3-4 weeks. It is important that the wound heal by first intention, so that the tissues are not swollen, the joints are not rigid. With a secondary suture, if the isolated ends of the tendon cannot be brought together without tension, the scar tissue formed between its ends can also be used to connect them (V. I. Rozov, 1952).
Tendoplasty of the extensor fingers is indicated in cases where there is diastasis between the ends of the tendon and functional disorders dependent on extensor injury. This is a planned operation. Various anatomical resources are used for extensor tendoplasty. A small diastasis between the ends of the tendon can be replaced with tendon bridges or part of the retinaculum extensorum. To replace extensive defects, the tendon of the long palmar muscle or a graft from the wide fascia of the thigh is used. To replace the defect of the long extensor tendon of the thumb, it is replaced with the tendon of the own extensor of the index finger or the tendon of the long radial extensor of the hand and homoplasty.
After suturing and extensor tendoplasty, the hand is fixed with a palmar plaster splint with a small layer of cotton-gauze lining. In case of damage to the extensor tendons at the level of the fingers, the splint is applied from the fingertip to the middle of the forearm, in case of damage to the tendon in the metacarpus - from the proximal interphalangeal joints to the elbow, in case of damage at the level of the wrist - from the metacarpophalangeal joints to the lower third of the shoulder, in a functional position on 20-25 days. The duration of immobilization depends on the extent of the wound, its course, the condition of the patient and other conditions.
With open injuries of the rear of the wrist or metacarpus, there is often a violation of the integrity of many extensor tendons. When performing a primary suture, it is sometimes necessary to open the corresponding bone-fibrous canal, the integrity of which must be restored at the end of the operation.
To avoid a soldered scar, the sutured tendon is covered with nearby soft tissues. On the back of the hand, intertendon jumpers are necessarily sewn together.
When the extensor tendon is damaged at the level of the metacarpophalangeal joint, the lateral bundles of the extensor apparatus of the finger are often damaged, which must be restored. Before sewing up the capsule, the joint should be inspected so that there are no small fragments of bone, cartilage or ligamentous apparatus left in it. The damaged capsule and ligaments are sutured with separate sutures.
N. M. Vodyanov, analyzing the results of the suture of the extensor tendons in 105 patients (143 tendons), depending on the nature of the wound and the location of the damage, cites the following data: when applying a tendon suture in the area of the fingers, out of 61, good results were obtained in 36, satisfactory - in 7 , poor - in 8, unknown - in 10. With a similar operation on the back of the hand out of 56, good results were achieved in 35, satisfactory - in 12, poor - in 1, and unknown - in 8. The author believes that the primary suture of the extensor tendons should be used in any conditions.
In the modern periodical literature, there are many reports of favorable functional outcomes of the suture and extensor tendon tendoplasty, and success in restoring the flexors of the fingers still often eludes surgeons. The average number of days of disability for open tendon injuries is 31.8 (see Table 12).
The problem of restoring the sliding apparatus of the extensors and flexors of the hand is still of interest to surgeons, although many of the specialists already have such significant experience that they have developed their own guidelines(N. M. Vodyanov, 1973; Ya. G. Dubrov, 1975; N. V. Kornilov, 1976; Pulvertaft, 1973; Wilhelm, 1975, etc.).
E.V.Usoltseva, K.I.Mashkara
Surgery for diseases and injuries of the hand

 A)
A) b)
b)