Antipyretics for children are prescribed by a pediatrician. But there are emergency situations for fever when the child needs to be given medicine immediately. Then the parents take responsibility and use antipyretic drugs. What is allowed to give to infants? How can you bring down the temperature in older children? What medicines are the safest?
In this article:
Deformation chest in children is a serious congenital or acquired pathology. It occurs in 2% of babies. Depending on the degree of the disease, the child may develop functional disorders work of the heart and respiratory organs.
Causes of deformation
Most often, the cause of improper formation of the chest is genetics. That is, while still in the womb, the fetus receives a program that is responsible for the abnormal development and growth of the cartilage of the chest. Fortunately, in many cases, congenital deformity of the chest in a child can be corrected if the child is treated in time.
Acquired chest deformity in a child occurs due to such serious diseases as bone tuberculosis, chronic pathologies of the respiratory system, scoliosis, as well as injuries and burns that occur in the sternum.
How does pathology manifest itself?
In 92% of children with congenital pathology of the chest, funnel-shaped deformity of the sternum is found. It is characterized by defective growth of the costal cartilages and a significant increase in the sternum in the transverse axis. As the child grows, the pathology becomes more pronounced, while the chest cavity decreases, which later becomes the cause of the curvature of the spine and disorders of the heart, blood vessels and respiratory organs.
Children with chest deformity, compared with healthy peers, lag behind in physical development, more often suffer from colds and broncho-pulmonary diseases, vegetative pathologies, and get tired more quickly during sports.
Types of pathology
Chest deformity is classified into the following types:
- Keeled deformation: chest protrudes forward like a keel from a boat. Commonly called "chicken breast".
- funnel-shaped: chest looks too sunken, as if pressed inward. The second name is "shoemaker's chest".
- flat: the sternum and ribs are flattened towards the anteroposterior axis.
- congenital cleft chest: the sternum is as if split into two parts.
- arched: Currarino-Silverman syndrome, rare.
- Rib-muscular anomaly: this is a complex pathology of bone tissue, affecting not only the chest, but also the spine, muscular apparatus and other organs.
The degree of severity of the deformity varies: in some children, a small cosmetic defect can be noted that does not require serious correction, while in others, a pronounced pathology.
In modern traumatology, there are 3 degrees of chest deformity:
- 1 degree. The depth of the funnel-shaped recess is not more than 2 cm. The displacement of the heart is not detected.
- 2 degree. The depth of the funnel is from 2 to 4 cm. The heart is displaced up to 3 cm.
- 3 degree. The depth of the funnel is from 4 cm. The displacement of the heart is more than 3 cm.
2 and 3 degrees of chest deformation in a child are characterized by pathological pressure of the sternum on the lungs. This is fraught with the development of chronic broncho-pulmonary diseases - bronchitis, pneumonia, etc.
Diagnostic methods
A physical examination by a pediatrician makes it possible to detect changes in the shape, symmetry and circumference of the chest in children, wheezing in the lungs, heart murmurs, etc. Often, when examining such children, dysembryogenetic stigmas are diagnosed: increased joint mobility, gothic sky, etc. Available signs deformed structure of the chest require mandatory consultation with a thoracic surgeon, orthopedist and traumatologist.
Thoracometry diagnoses the degree and type of deformity, assesses the depth and width of the chest, refines thoracic parameters and monitors them in dynamics. CT scan and chest x-rays of children provide more accurate data on existing changes in the sternum, ribs and spine. With their help, the bone structure of the chest is assessed, the presence of pathological changes in the lungs, displacement of organs in relation to each other.
Treatment
Treatment of chest deformity in a child is carried out under strict control by an orthopedist. The keeled pathology of the sternum does not require specific therapy, since it does not interfere with full-fledged work internal organs. In this case, children may experience only slight fatigue and shortness of breath. The defect is easily eliminated by thoracoplasty.
Conservative therapy is carried out with a sunken chest. The course of treatment depends entirely on the degree of retraction of the sternum. Grade 1 and 2 require therapeutic exercises, with the emphasis on the sternum: the patient learns to do push-ups, spread the dumbbells to the sides, and pull themselves up. Also, the child is shown to engage in sports such as rowing and volleyball - the loads resulting from these exercises prevent further retraction of the sternum. The result is a quality massage.
In severe cases, a surgical operation is prescribed, but it can be performed no earlier than the child reaches 7 years of age. The fact is that at this age the pathology ceases to form. During the operation, the doctor makes an incision in the child's chest and inserts a magnetic plate there. After the operation, a special belt with a magnet is put on the outside of the chest. They begin to attract each other, a gradual healing effect occurs - usually a sunken chest changes after 2 years of wearing magnetic plates.
If the chest defect is due to heredity, then initially the child is examined for possible pathologies that could cause this deformity, and then treatment is carried out - conservative or surgical, depending on the underlying cause of the disease.
Prevention
Preventive measures include the following recommendations:
- Regular medical check-ups.
- Timely treatment of diseases respiratory systems s.
- Avoidance of injuries and burns of the chest.
- Sports, sufficient physical activity of the child with training of the abdominal muscles, spine, back.
- Healthy food.
The sooner a chest deformity is diagnosed in a child, the more successful and easier the treatment will be. In addition, on initial stage diseases can be cured pathology without resorting to surgical treatment.
Useful video about chest deformity
Keeled deformity of the chest
Definition and pathogenesis
Keeled deformity of the chest (KDHK) is characterized by a symmetrical or asymmetric curvature of the anterior sternum and ribs articulating with it. KDHK causes only a cosmetic defect in children; functional examination does not reveal any deviations from age norms. However, in adolescents and adults, CDHC can cause functional disorders(decrease in vital capacity of the lungs, increase in minute volume of breathing, decrease in oxygen consumption coefficient, etc.), due to a decrease in the mobility of the ribs, the presence of the entire sternocostal complex in a state of "constant inspiration".
KDGK classification
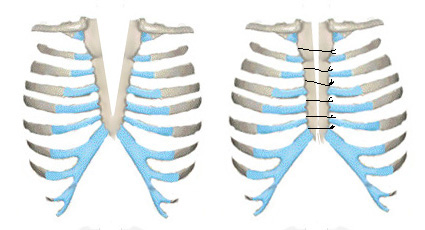
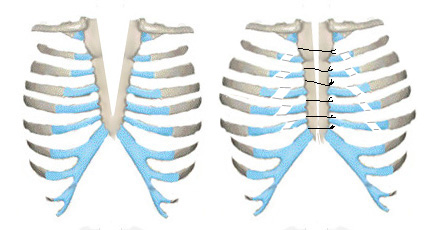
There are several classifications of KDGK, the most complete and practically significant of which was proposed by G.A. Bairov and A.A. Fokin. They distinguish three types of CDGC: manubriocostal, corporocostal, and costal. The manubriocostal type is characterized by forward bending of the manubrium of the sternum and 2-3 costal cartilages that articulate with it. The body of the sternum and the xiphoid process are more often displaced posteriorly. In the corporocostal type, the sternum is either directed obliquely downward and forward in a straight line with a maximum protrusion in the region of the lower third, or arched forward in the region of the middle and lower third. The cartilaginous parts of the ribs are often curved inwards. The costal type is due to the forward bending of the costal cartilages. The curvature of the sternum is not expressed and is more often of a rotational nature.
Methods of treatment of KDHK
The vast majority of surgeons are of the opinion that the treatment of CDGC is only surgical. The methods of corset correction proposed by several authors with the help of "pressing" corsets are not widely used. Lester performed the first thoracoplasty for CDH in 1953. In our country, the first operation was performed by G.A. Bairov in 1967. Below we provide a description of the most well-known methods surgical treatment KDGK.
Thoracoplasty according to Ravitch M.
A transverse submammary skin incision is made. The rectus abdominis muscles are dissected from the sternum and costal arches. The large and small pectoral muscles are cut off from their attachment points on the chest. All costal cartilages are resected subperichondrially on both sides, starting from 2 including the costal arches. Catgut sutures are applied to the perichondrium remaining in the places of cartilage removal, wrinkling it into an "accordion". Thus, there is a shortening of the intercostal spaces and perichondrium, and the sternum descends to its normal position. With severe curvature of the sternum, a wedge-shaped sternotomy is performed. Parts of the sternum at the site of sternotomy are fixed with two U-shaped bone nylon sutures. On top of the sternum, in order to fix it in a corrected position, the pectoralis major muscles are sutured to each other along the midline. From below, the rectus abdominis muscles are sutured to them. The wound is sutured in layers.
Thoracoplasty according to N.I. Kondrashin.
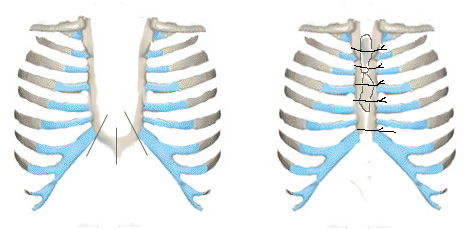
A vertical skin incision is made along the anterior surface of the chest from the handle of the sternum in the center of it and 4 cm below the xiphoid process. The xiphoid process of the sternum is cut off and, together with the rectus abdominis muscles, is taken downwards. Subperiosteally produce a transverse sternotomy between the I and II ribs. In the longitudinal direction, subperiosteally between the upper and lower sternotomy, a keel-shaped deformed body of the sternum is resected, leaving its lateral plates at the junction of II-VII ribs with the sternum. The II-VII ribs are dissected subperiosteally on both sides. After that, the crossed ribs are transposed together with the remaining plates of the body of the sternum to the center and they are sewn together with thick lavsan threads with interrupted sutures. Stitches are placed on the sternum, respectively, II-VII ribs. In this case, the ribs in the places of their dissection are not sewn together. The second ribs are fixed with two interrupted thick lavsan sutures to the remaining part of the sternum handle (Fig. No. 1).
A B C
Rice. No. 1. Scheme of thoracoplasty operation according to N.I. Kondrashin with keeled chest deformity.
A) skin incision b) resection of the body of the sternum, dissection of the II-VII ribs on both sides; c) transposition of the crossed ribs together with the remaining plates of the body of the sternum to the center and stitching them together.
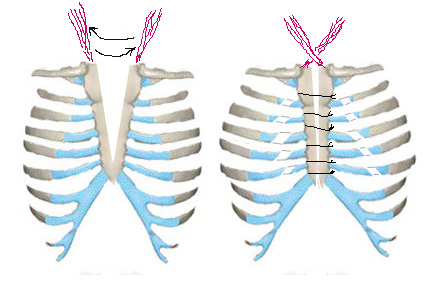
Thoracoplasty according to O.V. Dolnitsky and L.N. Dirdovskaya.
A wavy skin incision is made with an additional vertical one along the midline. The sternum and deformed costal cartilages are exposed throughout. The large pectoral muscles, rectus abdominis muscles, and sometimes the external oblique muscles are cut off from their place of attachment. The costal cartilages from 2-3 to 7 ribs on the right and left are excised subperchondrium. At the level of the 3rd-4th intercostal space, transverse sternotomy of the sternum is performed. Then the distal end of the sternum is resected within 1-1.5 cm, a triangular groove is formed at its end, where the xiphoid process is sewn with lavsan sutures. The tension of the rectus abdominis muscles causes the sternum to descend backwards. The large pectoral muscles are connected along the midline to each other, and the rectus and external oblique muscles of the abdomen are sutured to them below. Thus, a kind of muscular frame arises, putting pressure on the sternum from the front (Fig. No. 2).


a B C
Rice. No. 2. Scheme of thoracoplasty operation according to O.V. Dolnitsky and L.N. Dirdovskaya at KDGK.
a) skin incision; b) resection of costal cartilages, transverse sternotomy, shortening of the distal end of the sternum; c) fixation of the sternum, suturing of the pectoralis major, rectus and external oblique muscles of the abdomen.
Thoracoplasty (metallosternochondroplasty) according to V.A. Timoshchenko.
The operation is performed with corporal and costal forms of CDGC. A transverse submammary skin incision is made from the left nipple line to the right. The xiphoid process is cut off from the sternum. In a blunt way, the parietal pleura is exfoliated retrosternally on both sides. The pectoral muscles are stratified, exposing only the deformed costal cartilages. The latter subperichondrially resect. The costal arches are cut off from the sternum. A transverse wedge-shaped sternotomy is performed to correct its deformity. For reliable fixation of the sternocostal complex in a corrected position, a titanium plate is installed in front of the sternum, which is bent individually according to the shape of the patient's chest and fixed to the bone part of the ribs. The costal arches are fixed to the sternum with nylon sutures. The plate is removed after 6 months.
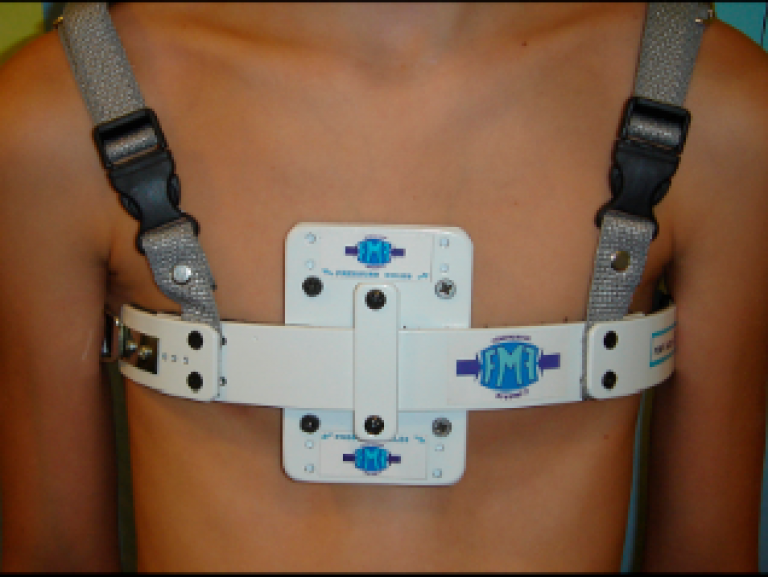
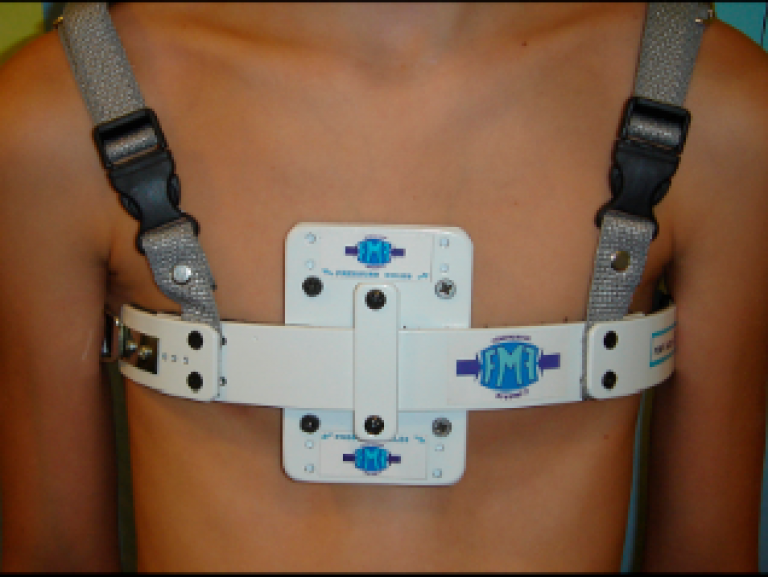
The use of an external "pressing" corset according to Haje SA.
The technique is based on the plastic properties of the sternocostal complex in children and consists in the gradual compression of the chest in the sagittal direction with an external corset. The author describes the results of treatment of 21 patients under the age of 13, who were wearing a corset of the original design and, gradually reducing the length of the lateral rods, corrected the keeled deformity. The period of wearing a corset is up to 2 years.
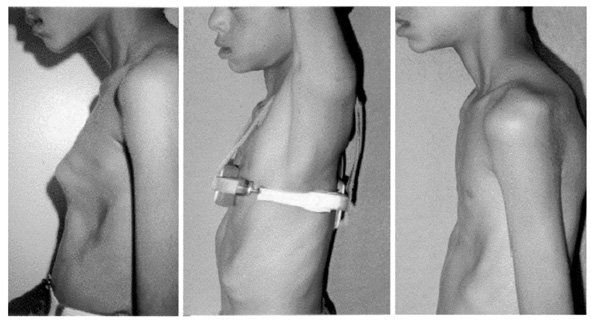
Rice. No. 3. The method of correction of KDGK according to Haje SA.
The vast majority of methods of surgical correction of CDGC are very traumatic, since they include manipulations on the osteochondral and muscle tissue chest. Many authors do not use any additional fixation devices to stabilize the sternocostal complex. The feasibility of using an external corset proposed by Haje raises some doubts, given the need to constantly wear a chest compression device for up to two years.
Rare congenital deformities of the chest
Rare congenital deformities of the chest include a rib-muscular defect (Poland syndrome), sternum defects (splitting and bifurcation of the sternum), Currarino-Silverman syndrome. There are isolated reports of these defects in the literature, and M. Ravith believes that they account for approximately 2% of all DHA.
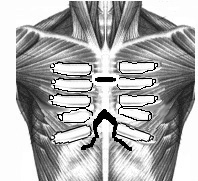
Rib-muscular defect - Poland's syndrome
Poland's syndrome (SP) is a complex of malformations, including the absence of the pectoralis major and minor muscles, syndactyly, brachydactyly, atelia (absence of the nipple of the breast) and / or amastia (absence of the breast itself), deformity or absence of several ribs, absence of hair in the axillary depression and a decrease in the thickness of the subcutaneous fat layer. Separate components of this syndrome were first described by Lallemand LM (1826) and Frorier R (1839). However, it is named after the English medical student Alfred Poland, who in 1841 published a partial description of this deformity. A complete characterization of the syndrome in the literature was first published by Thompson J in 1895.
SP occurs with a frequency of 1:30,000 - 1:32,000 newborns and in 80% of cases it is right-sided. With the left-sided variant, various manifestations of the reverse location of the internal organs are sometimes noted, from dextrocardia to the full form of situs viscerum inversus. Chest deformity in SP varies from mild hypoplasia to aplasia of the costal cartilages or entire ribs on the affected side.
Treatment of SP is a technically complex surgical intervention. It has three goals: to eliminate the defect of the ribs and restore the bone frame, to eliminate the retraction of the hemithorax, to create the correct anatomical relationships of soft tissues with the modeling of the nipple and mammary gland.
In 1961, Sulaama M. et al. cited 5 observations of SP. In 4 patients plasty was performed with rib grafts taken subperiosteally from the surrounding region with muscle plasty (Fig. 4). In one patient with a total absence of two ribs, after subperiosteal mobilization, the rib above the defect was cut at the proximal end, and the rib lying under the defect was cut at the distal end. The free edges of the ribs are bonded like a bridge over the defect (Fig. 5).
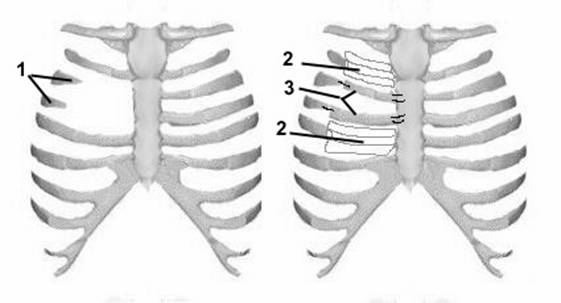
Rice. 4. Scheme of operation Sulaama 1 in case of Poland's syndrome.
1. - defect of the ribs, 2. - perichondrium remaining after resection of the cartilage, 3. - displaced autografts.
Rice. 5. Scheme of the Sulaama 2 operation for Poland's syndrome.
A. - view before surgery; b. - moving edges (the direction is shown by arrows); c - view after the operation.
Ravitch M. used Teflon-coated split rib grafts for reconstruction. Urschel HC used latissimus dorsi flaps in addition to rib grafts. Haller JA wrote that a complex deformity of the chest wall requires early intervention. childhood to replace missing ribs and eliminate the paradoxical movement of the anterior surface of the chest with the formation of a pulmonary hernia. To stabilize the chest wall, autogenous rib grafts and silicone prosthetic tissue were used to replace the missing endothoracic fascia. While restoring physiological functionality, this method absolutely does not eliminate the cosmetic defect due to the absence of the large and sometimes small pectoral muscles. However, the author himself notes that the use of silicone does not give good results in childhood and leads to a number of complications. According to the author, the only technique that allows to simultaneously eliminate the defect of the ribs and cosmetic defects is the use of rib autografts with simultaneous plasty with a part of the latissimus dorsi muscle. Three patients aged 10, 14, and 16 years old who were operated on using this technique had good results.
G.A. Bairov gave a description of 16 patients with SP operated on at the age of 4 to 11 years. Among his patients were 8 girls and 8 boys. Operation technique according to G.A. Bairov is as follows: an oblique incision through the place of maximum retraction along the intercostal space with an upward turn at the sternum exposes the sternocostal complex. Allocate the ends of the affected ribs. Bone grafts are cut out from the above and below the ribs, which, together with the periosteum, are moved to the site of the defect and sutured to the ends of the damaged ribs on one side and to the sternum on the other (Fig. 6).
Rice. 6. Scheme of surgery for Poland's syndrome according to G.A. Bairov
In 2 patients, in order to correct the deformity, traction threads were placed behind the ribs, which were fixed on the Marshev splint with a slight traction. In one patient with a large rib defect, a tibial allograft was used. The results of operations are recognized as good.
Congenital cleft sternum
Congenital cleft sternum (CCS) is a rare pathology. With this anomaly, there are usually no heart defects, the sternum is partially or completely split, and the pericardium, as well as the skin covering the sternum, is intact. A partial defect of the sternum is usually localized in its upper part and in the region of the handle, in contrast to thoracic and thoracoabdominal ectopia of the heart, in which the lower part of the sternum is predominantly split. In most patients with incomplete splitting of the sternum, its lower third and the xiphoid process are preserved. In addition to a pronounced cosmetic defect, the split sternum does not perform a protective function either. The anterior surface of the heart and the main vessels lie directly under the skin, which undoubtedly poses a certain danger to the life of the child, given the high level of childhood traumatism.
5 types of VRG are described in the literature (Fig. 7): 1. Splitting of only the manubrium of the sternum. 2. Splitting of the handle and the upper third of the body of the sternum (U-shaped). 3. Subtotal splitting of the sternum (V-shaped). 4. Total splitting of the sternum. 5. Splitting of the lower third of the sternum and the xiphoid process.
![]()
Figure 7. Types of cleft sternum according to G.A. Bairov.
There are two classic methods for closing a median defect. The Longino L method consists in midline suturing of the sternum rudiments after their partial marginal excision (Fig. 8). This operation is used in young children, when the chest is pliable, plastic enough, and the halves of the split sternum can be joined together without difficulty.
Rice. 8. Scheme of the Longino operation for CVD.
Thoracoplasty according to Sabiston differs from the previous one in that, in addition to partial marginal excision and suturing of parts of the sternum, parasternal oblique subperiochondral chondrotomy is performed to increase (expand) the size of the chest and prevent compression of internal organs (Fig. 9).
Rice. 9. Scheme of the Sabiston operation in VRH.
Along with this, there are a number of modifications. Knox L. with a U-shaped cleft proposed to resect the horizontal (lower) part of the sternum, and then lay it to increase strength on top of the newly formed sternum from two parts (Fig. 10). One patient was operated on using this technique with a good result.
Rice. 10. Scheme of the Knox L. operation in CVD. 1. - dissection lines of the horizontal branch of the sternum, 2. - autografts on the sternum.
G.A. Bairov published the result of surgical treatment of 11 patients aged from 1 month. up to 7 years old. Indications for surgery, according to G.A. Bairov are: paradoxical pendulum movements of the mediastinal organs, leading to circulatory disorders and venous congestion, respiratory disorders, lack of bone protection for the heart, lungs and main vessels, an increase in the defect with age, a cosmetic defect. In children under the age of 1 month of life, G.A. Bairov performs only stitching of the rudiments of the sternum according to Longino. At a later age, a Sabiston-type operation was performed, supplemented by clipping and cross-fixation of mm. sternoclaidomastoideus to the sternum (Fig. 11). Valla JS proposed, in addition to the first plasty method, to separate the periosteum from the connected parts of the sternum and fix it on the opposite side.
Rice. 11. Scheme of the operation according to G.A. Bairov at the VRG.
The main disadvantage when performing all the operations described above, especially in older children, is to some extent a decrease in the volume of the chest, especially with a significant diastasis between the parts of the split sternum. Simple mathematical calculations show that when a diastasis of 5 cm is eliminated, the volume of the chest in a 5-year-old child decreases by about 400 ml3. Although the undoubtedly high compensatory capabilities of the child's body help patients cope with increased intrathoracic pressure, it nevertheless complicates the course postoperative period. The sternum formed from split parts is thinner and less durable than normal. This circumstance definitely affects the functional result of treatment.
Currarino-Silverman Syndrome
The Currarino-Silverman Syndrome (SCS) consists of early synostosis between the constituent parts of the sternum. As a result, the sternum develops relatively smaller than normal. And as a result, there is a deformation of the entire bone frame of the chest, more often of the combined type (combination of keeled deformity of the sternum with retraction of the costal arches). The costal arches are longer than normal and approach the lower part of the sternum at a very acute angle. The xiphoid process is displaced posteriorly, towards the mediastinum. Sometimes this syndrome is combined with birth defects hearts.
The first description of the surgical correction of this type of DHA was given by Ravitch M. in 1952. He considered SCS as a variant of keeled chest deformity and proposed an original method for its correction. Since then, there have been few reports of this pathology in the literature. From 1966 to 1999, only three literature sources were found in the Medline database that describe this syndrome and methods for its surgical correction. Chidambaram B. described 5 patients with SCS and congenital heart disease. All patients had pronounced DHA. Unfortunately, in this article, the main focus is on the treatment of heart defects, without mentioning the correction of DHA at all. In the next article, Mehta AV also provides data on the treatment of heart defects in patients with SCS. And only in one article Shamberger RC, Welch KJ described 5 patients operated on for this syndrome. The authors used resection of costal cartilages from 2 to 7, transverse wedge resection of the sternum, followed by suturing the sternotomy incision with strong silk. No additional fixation of the sternum was performed. Long-term results are not described.
Acquired deformities
Acquired chest deformities (ACD) are curvature of the sternum and ribs that have arisen as a result of external influences on the child's body ( inflammatory diseases, trauma, surgery, etc.). Most often, this type of DHA is mentioned as a complication after thoracoplasty due to various kinds of congenital deformities and cardiac operations. It is noteworthy that all authors do not single out this type of DHA as a separate problem and the approach to their treatment is quite standard.
Deformities after purulent diseases of the chest cavity and chest wall
These deformations are a complication of running inflammatory processes caused by pathogenic microorganisms. Yu.F. Isakov et al described 15 patients with chronic empyema. All these patients had significant deformities of the chest, consisting in a sharp decrease in its circumference on the side of the lesion, narrowing of the intercostal spaces, and scoliosis of the thoracic spine. 4 of them also had rib deformities due to osteomyelitis. According to the authors, these 15 patients accounted for 2.8% of the total number of children with bacterial forms of lung destruction. This kind of DHA is currently extremely rare, due to the effectiveness of modern antibacterial drugs.
Post-traumatic deformities
Chest injuries are quite common in children. According to N.G. Damier chest injuries account for 3.4% of all injuries in children. Due to the mobility and softness of the bone skeleton, they can be easily corrected in the acute period of injury. Rib fractures in children rarely lead to DHA. More often, post-traumatic deformities occur after fractures of the manubrium and body of the sternum. Such DHA rarely lead to significant cosmetic defects and most often do not require surgical correction. However, Norotte G describes a 14-year-old patient with a transverse fracture of the body of the sternum, who, two months after the injury, developed a deformity of the chest in the type of VDHK. For which he underwent corrective surgery.
Relapses after thoracoplasty for various types of congenital DHA
The occurrence of relapses is directly related to the degree of deformity, the presence of concomitant pathology, the age of the patients, the severity of the surgical intervention and the method of thoracoplasty. Given the rather frequent occurrence of congenital DHA, especially in combination with various hereditary syndromes(Marfan or Ellers-Danlos), the number of complications after their surgical treatment also remains at high level. Willital (1977), after performing 235 operations using the Paltia plate, when analyzing the results after 4 years, noted 25% of satisfactory and poor results. Oelsnitz (1976), examining 120 patients operated on according to the classical Rehbain technique in the long-term period, noted good results only in 83 (69.2%). Satisfactory and poor results (30.8%) were due to different degrees of deformity relapses. Sbokos (1975) indicate recurrence of DHA after Rebine thoracoplasty in 15% of cases. It has been noted that if Kirchner wires are used to fix the sternum, relapses occur in 32% of cases (Dolnitsky, 1978). Summarizing the literature data on the results of thoracoplasty with the use of metal fixators, it can be noted that satisfactory and poor results were obtained in 23.8% of cases. Krause and Papiow (1977) have the greatest experience in performing thoracoplasty with fixation of the sternum with bone grafts. The authors performed 87 surgeries in children aged 2 to 15 years. Long-term results were monitored in 33 patients, and only in 41% a good result was obtained. In 48%, a satisfactory result was noted. And 4 patients (3.5%) had a pronounced recurrence of the deformity. After thoracoplasty without the use of special fixatives, relapses also occur. Ravitch M. (1977) noted 20% of unsatisfactory results after his operations, Pena (1981) and Ottolenghi (1982) - 15% and 20%, respectively. Robicsek (1974) slightly modified the operation of Ravitch M., but nevertheless received 31% varying degrees relapses. Haller (1978) performed 254 operations using the Ravitch M technique. 32% had relapses of the deformity. And only 10 children underwent relapse correction. The summary data given in the literature show that after thoracoplasty without the use of fixators, recurrence occurs in 19.9% of patients.
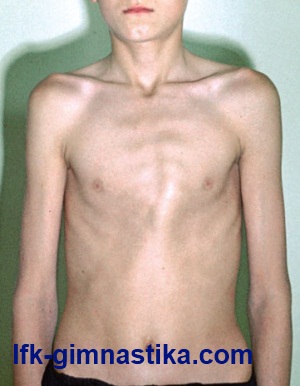
Keeled deformity of the chest ("chicken breast") is a congenital malformation, mainly found in individuals asthenic type physique (against the background of a disproportion in the growth of an abnormally developed sternum and costal cartilages) and progressing as the body develops, which subsequently often leads to the formation of a noticeable cosmetic defect. In some cases, pathology occurs in patients suffering from Marfan's disease, which, in addition, is manifested by arachnodactyly (lengthening of the limbs), dolichostenomyelia (tall growth), underdevelopment of fatty tissue, etc.
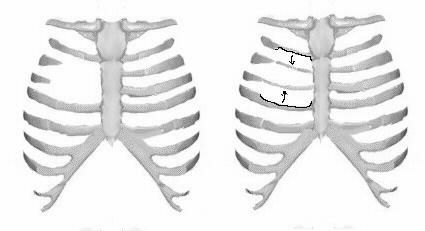
Clinically, with keeled deformity, a protruding sternum with ribs sinking along its edges is determined, which gives characteristic shape chest ("protrusion" of the chest). In the vast majority of patients, the retraction of the costal cartilages on the right and / or on the left from the fourth to the eighth pair of ribs is expressed. The edges of the costal arches, as a rule, are developed in a special way, the anteroposterior size of the chest is significantly increased and practically does not change during a respiratory excursion. In this case, the patient's chest is constantly in a state of inhalation.
In fact, the defect is detected from birth, becoming more and more pronounced with age. Functional disorders from of cardio-vascular system and respiratory organs during the first years of life are extremely rare - they are observed mainly in older children. Subjective complaints (fatigue, shortness of breath and palpitations during physical activity) and objective disorders (decrease in the vital capacity of the lungs and the oxygen consumption coefficient, an increase in the minute volume of breathing, etc.) are most pronounced in the presence of the aforementioned Marfan's disease. However, often the concern of the patients themselves is primarily due to cosmetic defect.
A fairly large number of classifications of keeled chest deformity have been proposed, but the most complete and practically significant of them is the one developed by G.A. Bairov and A.A. Fokin. According to their proposal, three types of this defect are distinguished: costal (forward bending of the costal cartilages against the background of unexpressed or rotational curvature of the sternum), manubriocostal (forward bending of the sternum handle together with two or three costal cartilages articulating with it and displacement posteriorly (often) of the body of the sternum with the xiphoid process), and corporocostal (sternum or obliquely directed forward and downward in a straight line, forming a maximum protrusion in the region of the lower third, or arched forward in the middle and lower third; the cartilaginous parts of the ribs here are mostly curved inwards).
The diagnosis is established on the basis of physical examination data. X-ray examination allows assessing the condition of the chest organs and establishing the severity of the developed deformity: the retrosternal space is usually enlarged, the heart is often teardrop-shaped and deployed along its axis. In the lateral projection, the sternum is presented as if by separate segments delimited from each other. If necessary, additional methods are prescribed (sonography, examination of the function of external respiration, electrocardiography, etc.). Then, based on the results obtained, a patient management strategy is developed.
Keeled chest is a type of chest deformity in which the shape of the chest resembles a boat keel or chicken breast. This deformity is genetic in nature and is, in fact, a cosmetic defect, with the exception of cases when there is a narrowing of the chest, which negatively affects the functioning of internal organs.
Classification of keeled deformities of the chest
The keel deformation can congenital And acquired
There are three main types of keeled deformation:
- Type 1 - costal. The sternum is elongated and protrudes forward. The xiphoid process exceeds the norm in size and protrudes into the chest cavity. The shape of the costal cartilages is not changed, the cartilages themselves, together with the sternum, protrude forward, which gives the chest the shape of a pyramid.
- Type 2 - manubriocostal. The sternum is underdeveloped, shortened and protrudes forward along with the xiphoid process. On the sides of the chest is pressed inward, which also enhances the effect of its protrusion forward. The ribs are curved and have a horizontal orientation. The muscles of the anterior part of the diaphragm are underdeveloped. Also, with this type of deformity, prolapse of the heart can be diagnosed.
- Type 3 - corpus-costal. The sternum is shortened and distributed in breadth, and also protrudes significantly forward. The ribs (from the second to the fourth) protrude forward in the form of an arc. The pectoralis major muscles are attached outwards.
According to the structure of the chest, a keeled defect occurs symmetrical And asymmetrical.
Reasons for development
One of the main reasons for the formation of a keeled chest defect is a genetic predisposition. Such a pathology is not always evident in early childhood - in some cases it is diagnosed only after a few years, since with age the bones of the child become harder and the deformation is more pronounced. In addition, congenital keeled deformity of the chest may be accompanied by a number of other defects, such as dolichostenomyelia or arachnodactyly.
Diseases of the skeletal system of the body can also affect the origin and development of such a defect. So, for example, scoliosis, kyphosis, a disease that provokes the accumulation of calcium salts in the ligaments of the spine (Bekhterev's disease), heart disease can provoke an abnormal development of the chest in the form of a "chicken breast".
Symptoms
Children with keeled deformity of the chest, as a rule, have an asthenic physique, and this makes the defect more noticeable. The chest is expanded, does not rise or contract when breathing, so it seems that the child is always in a state of inspiration.
The ribs from the 4th to the 8th sink down on one or both sides of the chest, their edges are turned outward.
Keeled deformation in mild form is a cosmetic defect, while the deformity in combination with Marfan's syndrome (developmental pathology connective tissue) can cause problems in the work of the heart, blood vessels and lungs, shortness of breath and fatigue.
Diagnostics
During the examination, the orthopedist draws attention to the external manifestation of the defect and directs the patient to additional examinations:
- X-ray examination. Allows you to clarify the degree and severity of deformity, to identify the presence of diseases of the spine.
- Computed tomography and magnetic resonance imaging. It is used to determine the presence or absence of changes in the internal organs of the chest (heart, lungs), as well as to identify concomitant complications.
- Consultations and examinations in the field of cardiology and pulmonology. As a rule, the patient is assigned an ECG to detect abnormalities in the work of the heart and spirometry to examine the lungs.
- Spinography. With the help of this method of research, the presence of a pathology of the development of the spine, as well as its degree, is determined.
Treatment
There are two ways to treat a keeled chest defect:
- conservative
- operational.
conservative treatment is used in the early stages of deformity development and only in early childhood. The fact is that in the early stages of development, this deformation is in the nature of a cosmetic defect, without affecting the functioning of internal organs. In children, bone tissue is more flexible and elastic than in adults, so conservative treatment can bear fruit.
Procedures included in the conservative treatment:
- Massage.
- Healing Fitness.
- A course of anti-inflammatory and analgesic drugs.
- Ferret compression system.
These methods of treatment are aimed at improving the functioning of the circulatory system, metabolism, strengthening the muscles of the chest, which will undoubtedly improve the aesthetic appearance of the chest.
Operational treatment is prescribed in two cases:
- if the patient has an unstable emotional state against the background of a psychological complex, and he is convinced that only an operation will help eliminate the defect and restore the normal shape of the chest (however, doctors do not recommend performing such an operation without good reasons);
- if the pathology negatively affects the work of the internal organs of the chest, preventing their normal appearance and functioning and causing serious diseases of the heart, blood vessels and lungs.
Currently, to eliminate the keeled chest deformity, the following are used:
- A minimally invasive intervention (Abramson's technique), in which two small incisions are made on the sides of the chest, through which two metal plates are attached to the ribs. One large plate is attached to these plates, which allows you to straighten the defect. This design is removed after a few years.
- Open access surgery (Ravich method), in which the skin under the mammary glands is cut, and the pectoral muscles are separated from the ribs. Then the rib cage is brought into a physiologically correct position by suturing the perichondrium and reducing the intercostal spaces.
After the operation, a recovery period follows, during which it is recommended to undergo a course of massage, exercise therapy and physiotherapy.
Chest deformity
is a congenital or acquired change in the shape of the chest. The term "thorax" means - the musculoskeletal frame of the upper body, which protects the internal organs. Deformation of the chest has an inevitable effect on the heart, lungs and other organs located in the chest cavity, causing a violation of their normal activity.
The cause of various deformities of the chest is the abnormal development of the cartilage of the ribs and sternum. In most children, such anomalies are already noticeable at birth, and in some cases become visible in late childhood. A defect in the connection of the right and left rudiments of the sternum in the process of embryonic development leads to the fact that a cleft is formed in the upper or lower part of the sternum. The sometimes observed cleft of the entire sternum is combined with protrusion of the pericardium or the whole heart, as well as with severe congenital heart defects.
Congenital and acquired chest deformities occur in 4% of the population. Depending on the degree of its severity, many types of deformities of the sternum and ribs cause functional disorders in patients in the cardiovascular and respiratory systems. Due to bone and cartilage defects, the protective and frame functions of the chest are reduced. As a result of cosmetic deficiencies, pronounced psychological disorders develop in children, children become withdrawn into themselves, shun their peers. These circumstances adversely affect the harmonious development of the child's body and the social adaptation of patients.
Children who have a pronounced chest deformity, as a rule, have a reduced systolic arterial pressure and increased diastolic, and they also have increased venous pressure, which has a very adverse effect on blood circulation. As a result, children quickly get tired, are asthenized, and often lag behind in physical development. However, with each degree of chest deformity, the child's condition can be compensated, subcompensated and decompensated, depending on the individual characteristics of the body, growth rate, stress and concomitant diseases.
Depending on the localization of the deformity of the chest, a violation of the shape of the anterior, posterior and lateral walls of the chest is distinguished. Moreover, the severity of the deformation can be different: from an almost imperceptible cosmetic defect to a gross pathology that causes disruption of the heart and lungs.
As mentioned above, all chest deformities can be divided into two groups: congenital (dysplastic) and acquired. As a rule, congenital deformities are less common than acquired ones.
Acquired chest deformities develop as a result of various diseases, such as chronic diseases lungs, bone tuberculosis, and they can also develop due to injuries and burns of the chest area.
Congenital deformities of the chest due to underdevelopment or anomalies in the development of the spine, ribs, sternum, shoulder blades and chest muscles. The most severe deformities are observed in violation of the development of bone structures. Congenital deformities of the chest, as a rule, are characterized by a change in the shape of the anterior surface of the chest.
The most common congenital chest deformities are funnel chest, flat chest, and keeled chest. Funnel chest deformity.
Funnel chest deformity.
Funnel-shaped chest (or as it is also called - "shoemaker's chest") is breast deformity, characterized by the inferiority of the costal cartilages, resulting in a depression in the middle and lower chest. It is the most common malformation of the sternum (accounts for 91% of all congenital deformities of the chest). The chest is enlarged in the transverse direction, there is a bulge () and lateral curvature in thoracic region spine. As the child grows, the deformities become more pronounced. Growing ribs seem to tighten and press the sternum inward. In this case, the sternum shifts to the left and the heart and large vessels rotate somewhat. With this malformation, as a result of retraction of the sternum, a decrease in the volume of the chest cavity occurs. A pronounced violation of the shape of the chest leads to a curvature of the spine, displacement of the heart, as well as disruption of the heart and lungs, and changes in arterial and venous pressure.
It is assumed that funnel chest deformity occurs due to a genetically determined change in the normal structure of cartilage and connective tissue. Children with funnel-shaped breasts often have multiple malformations, and a family history reveals cases of a similar pathology in close relatives. In newborns and children younger age this deformation is hardly noticeable. Retraction of the ribs and sternum increases during inspiration (inspiration paradox). As mentioned above, as the child grows, the pathology becomes more pronounced and reaches a maximum by the age of 3. Children with this congenital pathology, as a rule, lag behind in physical development, suffer from vegetative disorders and frequent colds. In the future, this deformation of the chest becomes fixed. Gradually, the depth of the funnel increases, reaching 7-8 cm. The child develops scoliosis and thoracic kyphosis. A decrease in respiratory excursions of the chest by 3-4 times compared with the age norm is revealed. There is an increase in disorders of the cardiovascular and respiratory systems.
The funnel-shaped chest has three degrees of deformation:
With the first degree of funnel chest, the depth of the displacement of the sternum ("funnel") is within 2 cm, without displacement of the heart. In the second degree - the depth of deformation is not more than 4 cm, with a displacement of the heart by 2-3 cm. The third degree of funnel chest is characterized by a depth of deformation of more than 4 cm, as well as a displacement of the heart by more than 3 cm.
Treatment for pectus excavatum:
With this congenital deformity of the chest conservative therapy(exercise therapy, massage, etc.) is ineffective. Minor deformities that are not accompanied by a noticeable impairment of cardiorespiratory function can be left for observation without surgery. With the second and third degrees of deformity, surgical reconstruction of the chest is indicated in order to create normal conditions for the functioning of the heart and lungs. Operations are carried out when the child reaches the age of 6-7 years. There are many ways surgical treatment However, it should be noted that traumatologists manage to achieve the desired result only in 40-50% of patients. Radical intervention is aimed at increasing the volume of the chest cavity. For this purpose, after mobilization of the sternocostal complex, a special stainless steel plate (strut) is installed behind the sternum and fixed to the fourth or fifth rib on each side. After 6 months or later, the spacer can be removed.
Recently, for the treatment of funnel chest, the method of two magnetic plates is used, which consists in the fact that one plate is implanted behind the sternum, and the second is placed outside on a special corset. The outer magnet pulls the inner plate anteriorly, thus gradually eliminating the deformity of the patient's chest.
 Keeled deformity of the chest.
Keeled deformity of the chest.
Keeled chest ("chicken chest") is a congenital deformity of the chest, characterized by protrusion of the sternum and ribs forward, an increase in the anteroposterior size. This pathology is caused by excessive growth of costal cartilages. Usually the cartilages of the fifth or seventh ribs grow. With a keeled chest, the sternum protrudes sharply forward, the ribs approach it at an acute angle, giving the chest a characteristic keel shape. This deformity of the chest is often congenital, although it may be acquired as a result of rickets, bone tuberculosis, etc. As a rule, this type of deformity occurs in children 3-5 years of age. As the child grows, the violation of the shape of the breast becomes more pronounced, a significant cosmetic defect occurs. The heart takes the form of a drop (the so-called "hanging heart"). This type of deformation is relatively rarely accompanied by dysfunction of the lungs and heart. The origin of this type of malformation is associated with genetic anomalies that adversely affect the differentiation of tissues during the period of bryogenesis of the fetus. As a result of this, dysplasia of the chest tissues and an anomaly in the structure of the diaphragm occur. In patients with keeled chest deformity, the anterior part of the diaphragm is absent, and the lateral areas attached to the seventh-eighth ribs are hypertrophied. This leads to retraction of the lateral sections of the chest and protrusion of the sternum anteriorly, as well as to a decrease in the volume of the chest. With age, the changes progress, resulting in a gradual increase in compression of the internal organs, which in turn is a consequence of dysfunction of the lungs and the cardiovascular system.
The keeled deformity of the chest causes only a cosmetic defect in children; a functional examination does not reveal any deviations from age norms. However, in adolescents and adults, this type of deformity can cause functional disorders, for example: a decrease in lung capacity, an increase in respiratory minute volume, a decrease in the oxygen consumption coefficient, etc. These disorders occur due to a decrease in the mobility of the ribs, as well as the location of the entire sternocostal complex in state of "permanent inspiration". As a rule, patients with a keeled chest complain of shortness of breath, fatigue, palpitations that occur during exercise.
As for treatment, surgical intervention for keeled deformity of the chest is indicated only if the functions of the internal organs are impaired.
Types of surgical intervention for keeled chest deformity: Abramson's operation (minimally invasive correction, analogue of the Nass operation) and sterno-chondroplasty operation (an analogue of Ravich's operation). Minimally invasive correction methods using endoscopic techniques are also being developed, the purpose of which is to avoid incisions on the chest wall. During the operation, the curvature of the sternum, the deformation of the ribs, as well as the correction of the costal cartilages are eliminated. As a rule, the operation is not performed on children under 5 years of age. Also, in childhood, conservative treatment with the use of orthoses (corset) is possible, and recently the most effective method the use of a dynamic compression system according to Ferret is considered.
Flat chest deformity.
A flat chest is the result of a particular physique. With this deformation of the chest, a decrease in the anteroposterior dimensions of the chest in volume is observed without disturbing the functions of the heart, lungs, and blood vessels. It should be noted that a flat chest is not a disease, but a development option. As a rule, no treatment is required.
The following deformities are also referred to congenital deformities of the chest:
- arched chest
- congenital cleft sternum
- Poland's syndrome
Arched sternum is the rarest type chest deformities. Otherwise, it is called the upper keel or Currarino-Silverman syndrome. With this type of chest deformity, a protruding groove forms in the upper part of the chest, formed by early ossification of the sternum in the region of the Lewis angle (the articulation of the handle and the body of the sternum) and overgrown cartilages of two ribs, while the other part of the chest looks normal. In some cases, a convex sternum may be combined with a moderate funnel-shaped deformity in the lower part of the sternum, however, this deformity cannot be corrected. This chest deformity is purely cosmetic. Correction is possible by sterno-chondroplasty according to the type of Ravich operation, with or without simultaneous osteosynthesis.
Congenital cleft sternum is a congenital disorder. According to statistics, it occurs in 2% of people. A patient with this pathology has a partially or completely split sternum. This pathology is serious, it is not only an aesthetic defect: with a cleft chest, the anterior surface of the heart and the main vessels are not protected by the chest, but are located immediately under the skin. The only way to treat cleft breasts is surgery. The type of surgery depends on the age of the patient.
In children under the age of 1 year, the following method of surgical intervention is used: the sternum is partially excised and sutured along the midline. However, the halves of the breasts are joined together only while the child is very small and the bones retain some flexibility. Therefore, in older children, from 1 to 3 years old, the following method of operation is used: the operation begins in the same way, with partial excision of the sternum, and then expansion of the chest is performed. This is achieved by filling the discrepancy between the segments of the sternum with costal autografts. For reliable fixation of autografts, as well as to prevent subsequent retraction of the sternum and possible deformation of the internal organs, a titanium plate is placed behind the sternum.
Poland's syndrome or rib-muscular defect is a genetic pathology, and if one of the parents suffers from this syndrome, the child is also likely to have the same syndrome in 50% of cases. Poland's syndrome affects all structures of the chest wall: sternum, ribs, muscles, subcutaneous fat and spine.
In view of the need for a comprehensive restoration of the chest, Poland's syndrome is treated only with the help of surgery. However, one operation is often not enough. First, the rib defect is eliminated, the bone deformity is restored, due to which the protective properties of the chest are restored. The purpose of the second operation is to improve the cosmetic result. This operation consists in modeling the mammary gland (endoprosthetics of an underdeveloped mammary gland in a woman and the pectoralis major muscle in men), as well as muscle plasticity. In many cases, Poland's syndrome is associated with short and fused fingers on the affected side (called brachysyndactyly), which requires the assistance of an orthopedic or reconstructive surgeon who has considerable experience in this field.
In general, it can be said about the treatment of chest deformities that conservative methods of treatment (massage, exercise therapy, sports, swimming) in this case are usually ineffective. In order to diagnose changes in the heart and lungs, which are caused by deformation of the chest, the patient conducts a whole range of examinations, which include: X-ray of the lungs, echocardiography, ECG, etc.



